legal resources necessary to hold negligent facilities accountable.
Peoria Nursing Home Abuse Lawyer
 Nursing home residents are unfortunately susceptible to various forms of abuse, from physical maltreatment to emotional neglect. This abuse not only causes immediate harm but can also lead to long-term psychological and physical deterioration.
Nursing home residents are unfortunately susceptible to various forms of abuse, from physical maltreatment to emotional neglect. This abuse not only causes immediate harm but can also lead to long-term psychological and physical deterioration.
At Nursing Home Law Center, LLC, our team of nursing home abuse lawyers is well-versed in these complex and sensitive cases. We strive to provide top-tier legal representation, ensuring victims receive the justice and support they need.
Understanding Nursing Home Neglect and Abuse in PeoriaAbusive behavior and negligence in Peoria represent significant issues that impact the most vulnerable members of our community. Our nursing home abuse attorneys are committed to addressing these concerns, providing legal support and advocacy for affected nursing home residents and their families. Understanding the nature and extent of abuse in nursing homes is essential for effective legal intervention.
The scope of abusive behavior in Peoria is broad, encompassing various types of mistreatment. Our legal team specializes in identifying and addressing these abuses, ensuring that affected individuals receive the justice and compensation they deserve. We prioritize the safety and dignity of residents, striving to uphold their rights and well-being.
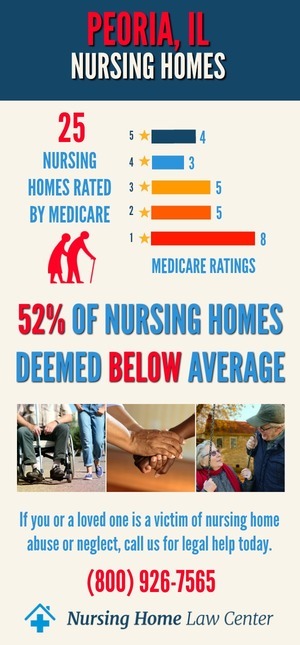
Nursing Home Statistics in Peoria, IllinoisThe Centers for Medicare and Medicaid Services (CMS) January 2024 updated data findings revealed a concerning situation where 15 out of the 28 facilities assessed, representing 54% of the total, received ratings categorized as "below average" or "much below average" by CMS.
Facilities Cited for AbuseAmong these nursing facilities with below-average ratings, some were subjected to additional scrutiny by inspectors who identified instances of abuse and neglect. It is crucial to bring attention to these facilities to ensure the safety and well-being of their residents. The following Peoria, Illinois, nursing homes were cited for abuse:
- Aperion Care Peoria Heights
- Sharon Health Care Elms
- Sharon Health Care Pines
- Sharon Health Care Willows
- Snyder Village
- Washington Senior Living
Neglect and abuse in nursing homes, a prevalent issue in Peoria, often lead to severe consequences for elderly residents. Recognizing abuse is crucial, as it can significantly affect residents' health and quality of life.
Definition and Types of AbuseAbuse represents a severe violation of the trust and responsibility bestowed upon care facilities. Recognizing these forms is the first step in addressing and preventing their occurrence.
Mistreatment in Peoria manifests in various forms, each detrimental to the well-being of residents:
- Physical Abuse: This type of abuse involves the deliberate application of force that results in bodily harm, discomfort, or pain to the resident. It may include hitting, slapping, pushing, or other acts that cause physical injuries.
- Sexual Abuse:Sexual abuse includes any non-consensual sexual contact or interaction, ranging from unwanted touching to more severe forms of sexual assault or battery.
- Emotional Abuse: Actions that inflict mental pain or distress constitute emotional, psychological, and verbal abuse. This can be verbal or non-verbal, involving intimidation, humiliation, isolation, or disregarding a resident's needs and feelings.
- Neglect: Neglect arises when a caregiving facility fails to provide the essential care and services necessary to maintain a resident's physical and mental health. This can include inadequate nutrition, leading to sudden weight loss, substandard hygiene, or ignoring the basic needs of the elderly.
- Financial Abuse: This occurs when a resident's financial resources or property are misused or exploited without their informed consent.Financial exploitation can involve the unauthorized withdrawal of funds, changing deeds or wills, or manipulating a resident into signing financial documents.
- Medical Malpractice: Substandard medical care that deviates from accepted medical practices, resulting in harm to the resident, falls under medical malpractice. This may include misdiagnosis, improper medication management, or neglectful medical treatment.
- Abandonment and Isolation: Forcing a resident into seclusion, restricting their social interactions, or leaving them alone without care or supervision can lead to significant psychological and physical decline and constitutes abandonment and isolation.
Each category of abuse not only infringes upon the rights of elderly residents but can also lead to severe, long-term consequences. It is imperative for caregivers, family members, and the community to remain vigilant and to take immediate action should any signs of these abuses be observed.
Identifying Signs of AbuseRecognizing signs of abuse and neglect is vital in protecting residents. Physical signs like bruises or unexplained injuries, along with behavioral changes such as withdrawal or fear, can indicate mistreatment. Prompt identification and action are crucial for safeguarding residents and preventing further harm.
All nursing facilities must carry adequate insurance and conduct proper background checks on all staff to minimize the risk of hiring individuals with a history of abuse.
The Role of a Nursing Home Abuse AttorneyOur law firm plays a critical role in advocating for the rights of victims and their families in nursing abuse cases. We provide comprehensive legal support, from investigating abuse claims to representing clients in court. Our dedication to justice and accountability drives our pursuit of fair outcomes for victims.
The process of holding nursing facilities accountable for abuse and neglect is a primary focus of our legal practice. We work tirelessly to ensure responsible parties are held liable for their actions, seeking justice and fair compensation for victims. Our team is committed to positively impacting the quality of care in nursing homes.
Common Injuries and Issues in Nursing Facility Abuse CasesFall-related injuries are a common concern in caregiving home abuse cases. Our legal team addresses these incidents, examining the circumstances leading to falls and advocating for affected nursing home patients. Ensuring the safety of caregiving home environments is a priority in our legal efforts.
Medical negligence, including medication errors and inadequate care, significantly impacts residents. We are experienced in handling cases involving medical negligence and working to secure justice and compensation for victims. Our focus is on improving medical care standards in nursing homes.
The Nursing Home Care Act: Protecting the Rights of Nursing Home ResidentsThe Nursing Home Care Act serves as a fundamental piece of legislation designed to protect elderly residents from elder abuse and neglect in nursing and assisted living facilities. It is a crucial safeguard for nursing home patients and their family members. The Act ensures that nursing home employees provide the proper care required by law.
Immediate Danger and Wrongful DeathThe immediate danger of harm leading to preventable death is among the most severe consequences of nursing home negligence. This Act obliges facilities to maintain standards that prevent such tragic outcomes, holding negligent parties accountable for their actions.
Legal Options for Nursing Home Abuse CasesWhen a nursing home resident falls victim to abuse, the Act provides a clear pathway for families to seek justice. The Act empowers nursing home abuse attorneys to pursue wrongful death cases or other legal actions against the responsible parties in cases such as:
- A resident has been sexually abused
- The patient has suffered unexplained bruises
- An individual has been subject to repeated problems
The National Center on Elder Abuse highlights that older adults are at a higher risk for mistreatment, especially in institutional settings like nursing facilities. Prevalent issues such as understaffing can lead to neglect, making it imperative for elderly people and their families to understand their legal options under the Nursing Home Care Act.
Why Choose Our Law Firm for Nursing Home Abuse Cases in Peoria?Our law firm is a leading choice for handling nursing home negligence cases in Peoria, thanks to our extensive experience and proven track record. We offer expert legal representation tailored to the unique needs of each caregiving home abuse case. Our commitment to our clients drives our success in achieving positive outcomes.
We provide compassionate and comprehensive legal support to our clients. Understanding the emotional toll of abusive behavior, we approach each nursing home abuse case with sensitivity and dedication. Our firm is committed to offering personalized legal services that address the specific needs of our clients and their families.
Our law offices work with insurance companies to ensure elderly loved ones receive the compensation they deserve.
Steps to Take if You Suspect Nursing Home Abuse in PeoriaTaking immediate action is crucial if you suspect mistreatment in a Peoria nursing facility. Documenting evidence and reporting the abuse are essential first steps.
Reporting the abuse to relevant authorities and seeking legal counsel are vital actions. Our legal team advises families on these actions, ensuring that they are carried out effectively to protect the rights of their loved ones.
Our Peoria nursing home lawyers guide families through these steps, ensuring proper legal measures are taken to address the abuse. Families can report nursing home abuse or neglect to the proper authorities, including the following:
- Illinois Department of Public Health's Nursing Complaint Hotline
- Medicaid Fraud, Abuse, or Neglect
- Department of Human Services' OIG Hotline
- Senior HelpLine at (800) 252-8966 or (888) 206-1327 (TTY).
- Illinois Department of Public Health
Our nursing home negligence lawyers offer free consultations, providing families with valuable insights and guidance on proceeding with their cases.
Protecting the Rights of Illinois Nursing Home ResidentsOur law firm is dedicated to upholding the rights and safety of nursing home residents in Peoria. We advocate for enforcing nursing home patients' rights, ensuring that caregiving facilities maintain a safe and respectful environment. Our legal actions aim to improve standards of care and prevent future abuse.
The impact of legal action on caregiving facility standards is significant. Our efforts in pursuing legal cases against abusive nursing facilities led to improved practices and heightened awareness of nursing home resident rights. We are committed to creating a safer and more dignified living environment for all nursing home residents.
In the fight against nursing home negligence, Nursing Home Law Center, LLC stands as Peoria's guardian. Call our nursing home abuse lawyers at (800) 926-7565 to schedule a free consultation and empower your fight for fair compensation.
 Peoria County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Peoria County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
