The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Nursing Home Wrongful Death Lawyer
Experienced Law Firm Helping Families Seek Justice and Compensation for Preventable Death
Losing someone you love is a tragic, devastating experience. If you believe that the death of your loved one was a result of nursing home abuse or neglect, you need the help of an experienced nursing home wrongful death lawyer to seek compensation.
Nursing Home Wrongful Death Settlements
When families lose a loved one in a nursing home or other medical facility under preventable circumstances, pursuing a nursing home wrongful death lawsuit can be one way to get justice and accountability. While there isn’t necessarily a standard average wrongful death settlement, it can be helpful to know what you may be able to obtain from this type of nursing home lawsuit.
Below are some examples of nursing home wrongful death settlements and verdicts we’ve achieved for families in these tragic situations:
$12,800,000 nursing home lawsuit verdict in a wrongful death case involving untreated bedsores that led to the resident’s death. This helps cover funeral expenses and other costs.
$3,000,000 nursing home lawsuit settlement for the nursing home wrongful death of a man who developed fatal pressure sores after being admitted to a skilled nursing facility following hip replacement surgery.
$2,150,000 nursing home lawsuit settlement in a wrongful death case where a resident developed bedsores at the assisted living facility, leading to sepsis and eventual death.
$1,250,000 settlement for a choking-related wrongful death nursing home lawsuit that was resolved before going to court.
$4,000,000 nursing home lawsuit settlement for a wrongful death case involving a man who suffered a fatal fall during a hospital stay after hip replacement surgery, resulting in a subdural hematoma.
While no nursing home lawsuit settlement in a wrongful death case can replace a family member or life partner, holding responsible parties accountable can help families find closure and prevent similar incidents from occurring to other residents in the future.

What Is Nursing Home Wrongful Death?
Wrongful death is a legal term referring to a situation where someone’s death is caused by the negligent actions or intentional harm of another party. Nursing home wrongful deaths occur when a nursing home resident dies as a result of nursing home negligence or abuse by the facility or its staff.
To determine if a nursing home death qualifies as wrongful, several factors are considered.
How to Prove Negligence in Nursing Home Wrongful Death Cases
To successfully pursue a nursing home wrongful death case, four elements of negligence must usually be proven. These elements establish that nursing home employees acted in a manner that led to the tragic loss of life.
Duty of Care
The first element requires showing that the nursing home owed a duty of care to the resident. By accepting a resident into their nursing home facility, the nursing home agrees to provide a safe environment, proper medical care, and the basic necessities required for the resident’s well-being.
Breach of Duty
Next, it must be demonstrated that the nursing home breached its duty of care. Breaches occur when nursing home staff members fail to follow standard procedures, ignore a resident’s needs, or allow unsafe conditions to persist.
For example, the nursing home fails to respond to a resident’s worsening bedsores, despite clear signs that their condition is deteriorating. The resident dies as a result of an infection.
Causation
The third element focuses on causation, which means proving that the breach of duty directly caused or significantly contributed to how the resident died. This is often one of the trickiest aspects to establish, as it requires clearly linking the nursing home’s actions – or lack thereof – to the resident’s passing.
For instance, if the resident with bedsores suffers a fatal infection because staff failed to provide appropriate treatment, it would be argued that the infection and subsequent death resulted directly from the staff’s actions.
Damages
Lastly, damages refer to the tangible and intangible losses suffered as a result of the resident’s death. This can include medical bills for treatments prior to their passing, funeral costs, and emotional pain experienced by the victim’s family members.
Losing a loved one in such avoidable circumstances is always devastating, and while no legal action can bring them back, holding negligent parties accountable through a nursing home lawsuit provides an opportunity for closure and reassures others that their loved ones will be safer in the future.
What Are Common Causes of Wrongful Death in Nursing Homes?
Wrongful death in a nursing home or assisted living facility can happen for various reasons. The common causes of wrongful death in these settings are:
Falls and Broken Bones
Fall prevention is an essential responsibility in nursing homes. Staff should take appropriate measures to reduce fall risks in older adults, as they are more susceptible to severe injuries. A single fall can lead to broken bones, internal injuries, and other complications that may contribute to a resident’s nursing home death.
Neglect
Failing to meet a resident’s basic needs can have devastating consequences. From failing to provide proper hygiene routines to ignoring signs of distress, neglect can cause a rapid decline in health, sometimes leading to nursing home deaths.
Infections
Many infections in nursing homes are preventable with proper care and hygiene practices. When staff fail to isolate contagious residents, follow handwashing protocols, or maintain cleanliness in shared spaces, infections can quickly spread, putting vulnerable individuals at serious risk of nursing home wrongful death.
Medication Errors
Mistakes in administering medications, such as providing the wrong drug, incorrect dosages, or missing doses altogether, can have severe consequences. These medication errors may cause adverse reactions or exacerbate existing health conditions, sometimes resulting in a nursing home wrongful death.
Bedsores
Bedsores, also known as pressure ulcers, develop when residents are left in one position for extended periods. Untreated bedsores can become infected, causing pain and infections like sepsis, and ultimately contributing to fatal complications if not addressed.

Choking or Aspiration
Many residents require assistance during meals to ensure they can eat safely. If proper supervision is not provided, residents may choke or aspirate food or liquids, potentially leading to respiratory complications or death.
Wandering and Elopement
When nursing homes lack adequate safety measures, residents with cognitive impairments like dementia can wander off or leave the facility unsupervised. These situations put residents at risk of severe injuries, exposure to harsh conditions, or fatal accidents.
Physical Abuse
Residents may suffer intentional physical abuse and serious injuries from staff or other residents. Even unintentional excessive force, such as being too rough while assisting someone, can lead to health risks, worsening the resident’s condition, and potentially contributing to their death.
Dehydration, Weight Loss, and Malnutrition
Failure to provide proper nutrition and hydration can result in extreme weakness, organ failure, and significant health deterioration. Negligence in monitoring residents’ diets or fluid intake can lead to fatal consequences.
Failure to Diagnose
When staff overlook medical symptoms or delay seeking medical treatment, time-sensitive conditions may go untreated. These delays can worsen a resident’s health dramatically, turning treatable complications into life-threatening emergencies.
These issues highlight the importance of maintaining high standards of care to protect the safety and well-being of all residents.

What Standards of Care Do Nursing Homes Need to Follow?
Every nursing home is responsible for ensuring residents are cared for to the best of their ability. The standard of care is high, and when it’s not met, the nursing home can be held liable for negligence.
Duty of Care to Nursing Home Residents
Nursing homes are required to provide a high standard of care to residents. This is a legal and ethical obligation. The duty of care encompasses different parts of the resident’s well-being, including their physical and emotional health, quality of life, and safety. Responsibilities of the nursing home staff include:
- Protecting the residents from nursing home abuse and neglect
- Maintaining a safe and clean environment
- Providing residents’ health care and monitoring
- Ensuring proper nutrition and hydration
- Preventing and treating bedsores
- Administering medications correctly
- Implementing fall and elopement prevention strategies
- Offering social and recreational activities
- Respecting the residents’ dignity and rights
Breaching Standards of Care and Failure to Prevent Nursing Home Wrongful Deaths
When they can’t provide the level of care they’re supposed to, it can lead to the wrongful death of a resident. Common breaches of this duty of care include:
- Failing to implement proper infection control procedures
- Understaffing, which means inadequate supervision and care
- Ignoring or downplaying residents’ medical complaints
- Failing to train staff members properly
- Neglecting to keep the nursing home safe
To ensure that nursing homes are maintaining the level of care that they should be, and therefore preventing nursing home wrongful death, they should:
- Conduct regular health assessments and update care plans accordingly
- Have emergency response plans in place
- Implement medication management systems
- Monitor nutrition and hydration
- Conduct risk assessments and develop prevention programs
Regulatory and Legal Standards
It’s not just that nursing homes should abide by their ethical obligations, but they are also legally required to. State and federal regulations are in place to ensure that nursing home residents are safe and receive proper care. Some critical federal regulations are:
- The Centers for Medicare and Medicaid Services (CMS) sets forth regulations for programs that take Medicare and Medicaid.
- The Nursing Home Reform Act of 1987 establishes the basic standard of care and rights that nursing homes have to provide to residents.
Every state has its regulations in place. They can regulate things like:
- Staffing ratios
- Nursing home licensing and inspection procedures
- Staff training and qualification requirements
- Specific care protocols for certain medical conditions
Nursing homes can help prevent wrongful death by following all state and federal regulations. They have to:
- Report nursing home abuse and neglect, including unexplained injuries
- Maintain detailed records of care for every resident
- Develop and implement quality assurance and improvement programs
- Undergo periodic inspections by state and federal agencies
How Family Members Can Report Issues in Nursing Homes
If you or a loved one has experienced mistreatment or observed questionable practices in a nursing home, knowing how to report these issues is important. Several organizations are dedicated to addressing nursing home abuse, neglect, and violations within long-term care facilities.
Adult Protective Services (APS)
APS is the primary agency responsible for investigating cases of elder abuse and neglect, including wrongful deaths occurring in nursing homes. They work to protect vulnerable adults and can provide resources to ensure their safety.
If you suspect a resident is facing physical, emotional, or financial abuse, contacting the local APS can launch an investigation and connect those affected with support services.
The Centers for Medicare and Medicaid Services
CMS oversees Medicare and Medicaid certifications for nursing homes. This organization conducts regular inspections to ensure nursing homes and other care facilities are meeting certain standards.
If the care provided at a nursing home is insufficient or non-compliant with regulations, CMS has the authority to enforce corrective actions. Reporting to CMS can help address systemic issues or immediate dangers to residents.
Long-Term Care Ombudsman Programs
Ombudsman programs focus on protecting the rights of nursing home residents and ensuring their voices are heard. An ombudsman can assist in resolving complaints about mistreatment, living conditions, or lack of services.
They act as an advocate for the resident, working closely with both the individual and the negligent facility to find a resolution that meets the resident’s needs and respects their rights.
State Licensing Boards
Each state has a licensing board that monitors nursing homes to ensure they comply with state-specific regulations. These boards have the authority to investigate complaints, enforce penalties, and even revoke a negligent facility’s license if necessary.
Reporting a concern to the state licensing board can address issues with management, staffing, or operational practices that may not meet requirements.
Understanding how each of these organizations operates can help you make an informed decision when seeking assistance for nursing home-related concerns.
How to Identify Nursing Home Neglect and Abuse
One of the first steps in filing a nursing home wrongful death claim is establishing who is liable and if negligence played a role in the death. Negligence in these cases is usually due to not providing the expected standard of care. Signs of nursing home negligence and abuse include in a nursing home include:
- Sudden and unexplained weight loss
- Dry skin and other signs of dehydration
- Unexplained injuries or a rapid decline in health
- Frequent falls or accidents
- Development of bedsores and skin conditions
- Unsanitary living spaces
- Over or under-medicating residents
- Signs of financial exploitation
- Unexplained bruises, cuts, or broken bones
- Lingering infections that weren’t treated properly
- Signs of emotional distress or withdrawal
- Fear of a certain person in the facility or a desire to leave the facility
- Sexually transmitted diseases
If you notice any of these signs, it’s important to take legal action by documenting evidence, reporting concerns, and seeking legal help.
What Evidence Is Needed to Support a Wrongful Death Claim?
When filing a nursing home wrongful death case, proving that nursing home abuse or neglect occurred involves gathering thorough and convincing evidence. Examples of evidence that may help establish liability include:
- Medical records showing issues with treatment or care
- Testimony from medical experts, explaining how the expected standard of care was not met
- Nursing home facility policies or procedures that reflect improper or unsafe practices
- Interviews with nursing home staff, residents, and visitors to build a clearer picture of events
- Photographs of unsanitary conditions, injuries, or other unsafe environments
- Statements from witnesses, including the victim’s family members, other residents, or healthcare aides
Whether the nursing home failed to provide the standard of care on purpose or was negligent, proving the nursing home or specific staff members were negligent is vital in your nursing home negligence case. Gathering medical records is going to be one of the most important aspects of the case.
Grieving Family Members’ Legal Rights
Surviving family members whose loved ones passed away due to negligence or nursing home abuse have rights. Their rights in nursing home wrongful death cases vary by state, but generally, their rights include:
- Filing a nursing home wrongful death claim
- Right to financial compensation for damages incurred due to the nursing home wrongful death
- Right to information surrounding their loved one’s care and what led to their passing
- Having a thorough investigation of the events leading to the wrongful death
- Right to protection from retaliation from the nursing home or its staff members
- Right to representation from an experienced legal team
- Ability to choose a different care provider for any loved ones still within the facility
- Right to privacy
Hiring a nursing home wrongful death attorney will help family members navigate a wrongful death lawsuit to ensure they can hold the facility accountable.

How Nursing Home Abuse Attorneys Can Help Pursue Justice
A nursing home abuse lawyer will play a vital role when it comes to family members filing a nursing home wrongful death lawsuit and seeking justice. They have the experience, knowledge, and compassion to guide them through the legal process.
Elder abuse attorneys combine their knowledge and experience of elder, personal injury, and wrongful death law to succeed. Here’s how they can help:
Investigation and Evidence Collection
One of the roles a nursing home wrongful death attorney has is to help investigate and collect evidence for your nursing home negligence case. The process they take for investigating and gathering evidence will vary depending on the legal team you choose, but it generally involves:
- Collecting and reviewing all medical information and records from the nursing home and other medical facilities
- Speaking with witnesses at the nursing home about the incident and events leading to the nursing home wrongful death
- Consulting with medical experts who can provide testimony that proves the nursing home wrongful death was due to negligence on the part of the nursing home or specific staff members
- Going over facility records to see what procedures weren’t followed
- Reviewing all state inspection reports to see if the facility has a history of negligence
- Gathering physical evidence, like photos of the nursing home resident’s living conditions and injuries prior to the death
Legal Representation and Advocacy
Nursing home wrongful death lawyers are here to be your biggest advocates and protect your rights. Their responsibilities include:
- Thoroughly explaining your legal rights and options so you can make the best decision
- Representing the family in settlement proceedings
- Representing the family in court if the wrongful death lawsuit isn’t settled
- Filing the nursing home wrongful death suit and handling the paperwork that goes along with it
- Offering emotional support when they can
- Protecting the family’s rights and interests
- Handling communication between parties involved in the nursing home lawsuit
Negotiation With Insurance Companies and Litigation if Necessary
Your nursing home attorney will handle negotiations and litigation for you. Their responsibilities relating to your nursing home lawsuit include:
- Engaging in settlement negotiations to ensure you get the maximum compensation for the damages incurred
- Preparing for trial (if applicable) by preparing documents and witnesses and developing a strong legal strategy
- Having a strong courtroom presence and ensuring all legal proceedings are followed correctly
Steps to Take After a Nursing Home Wrongful Death Incident
It’s hard to think about anything but your loved one after their death, but if you feel like the nursing home is responsible due to negligence, knowing what to do after can be helpful.
Immediate Actions
After your loved one passes away, below are some of the things you’ll want to do sooner rather than later:
- Report the death and events leading to the wrongful death death to the nursing home administration, local law enforcement, your state’s department of health, adult protective services, and/or the state licensing agency
- Document everything you can about the incident and wrongful death
- Gather evidence, like an incident report from the nursing home and copies of all your loved one’s medical records
- Find someone to do an independent medical exam
Legal Consultation With a Nursing Home Lawyer
After you do the above, you’ll want to consult with a nursing home wrongful death lawyer who knows about wrongful death lawsuits and nursing home neglect.
The consultation is an opportunity for you to talk with a knowledgeable nursing home lawyer about wrongful death lawsuits. You can work together to develop the right strategy to hold the nursing home accountable.
What Damages Can Be Recovered in Fatal Nursing Home Abuse Cases?
When you file a nursing home wrongful death lawsuit, you can seek compensation for various damages. Some of the most common types of compensation sought include:
- Medical expenses for the medical bills incurred due to the illness or injury that led to the wrongful death of your loved one
- Funeral expenses and burial costs
- Loss of financial support that the loved one was providing to the family members before they passed away
- Loss of companionship or consortium, which is the loss of love and affection from the loved one
- Pain and suffering that the nursing home resident went through before their nursing home wrongful death
- Loss of services, which covers any services the resident would’ve been able to provide for their family before their wrongful death
- Mental anguish
- Counseling services for the surviving family
- Loss of inheritance
- Punitive damage in the case of severe nursing home negligence or intentional misconduct

How Much Can Family Members Recover in a Wrongful Death Suit?
According to Law.com’s VerdictSearch, payouts in nursing home negligence cases resulting in wrongful death range from $15,000 to $91,500,000. The average recovery is $4,694,860, while the median award is $1,000,000. These claims typically arise from fatal falls, untreated infections, severe bedsores, malnutrition, medication errors, or other preventable harm.
Several factors can influence the value of a wrongful death case, including:
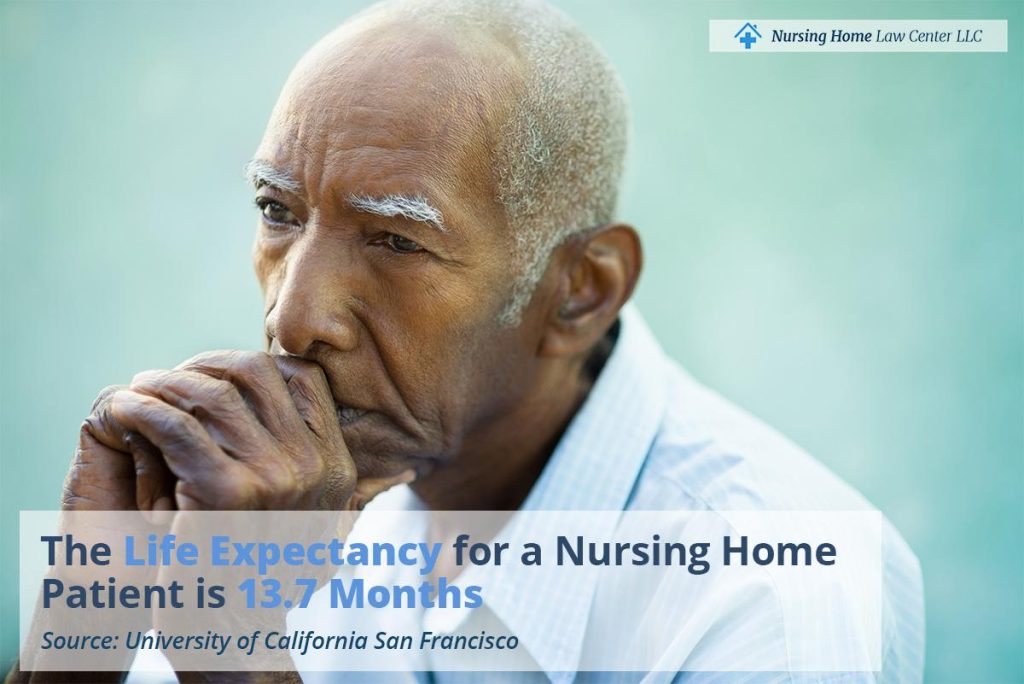
- Age, health, and life expectancy of the deceased resident
- Medical expenses, pain and suffering, and duration of decline before death
- Evidence of neglect (falls, untreated wounds, malnutrition, or sepsis)
- Documentation of care plans, fall risk assessments, and staffing levels
- Testimony from medical and nursing experts on causation
- Emotional and financial impact on surviving family members
- Potential for punitive damages if reckless or intentional conduct is proven
Example Nursing Home Wrongful Death Cases
$91,500,000 Verdict – Nursing Home Wrongful Death from Neglect and Dehydration
Dorothy Douglas, 87, entered a nursing facility for short-term care but deteriorated rapidly during her 19-day stay. Her family alleged she was left malnourished, dehydrated, and neglected due to chronic understaffing, leading to renal failure and death.
The defense argued her decline was caused by preexisting conditions, including Alzheimer’s disease, and pointed to records showing minimal weight loss. The jury found the facility liable for negligence, fiduciary breaches, and violations of the Nursing Home Act, awarding Douglas’ estate and family $91.5 million, including $80 million in punitive damages.
$50,000,000 Verdict – Undiagnosed Gallbladder Condition Leads to Wrongful Death
Toni Meredith, 57, admitted for rehabilitation following Guillain-Barré Syndrome, allegedly received no physical therapy during her nine-month stay. She later suffered repeated gallbladder attacks that went undiagnosed for months despite worsening symptoms. Her family argued that severe understaffing and delayed medical evaluations caused her fatal complications.
The defense maintained her decline was unrelated to negligence. The jury awarded $50 million in compensatory damages, but due to a high-low agreement, the estate ultimately recovered $5 million. Jurors later stated they were prepared to award an additional $100 million in punitive damages.
How Long Do I Have to File a Nursing Home Wrongful Death Lawsuit?
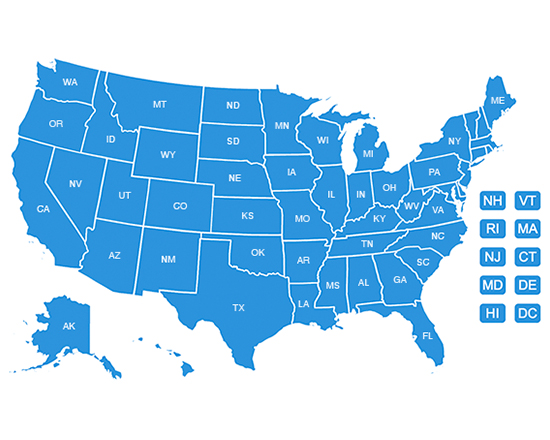
Most legal cases – criminal and civil – including nursing home wrongful death, have a statute of limitations on them. The statute of limitations for filing a wrongful death lawsuit varies from state to state. Ensuring that you file your elder abuse lawsuit within your state’s timeframe is key to seeking justice and compensation.
Generally, the statute of limitations for a nursing home wrongful death lawsuit is two to three years, but it’s important that you check with your state. Given the variables that can impact your wrongful death lawsuit, it’s important to take legal action immediately to ensure that no one gets away with negligence.
Book a Free Case Review With Our Law Firm
Losing a loved one is never easy, especially when it’s because of the negligence of the nursing home that was supposed to take care of them. While nothing will bring back your loved one, filing a nursing home wrongful death lawsuit can help you get compensation for your loss, hold the nursing home and staff members accountable, and give you a sense of justice.
Working with a who understands how to handle nursing home wrongful death lawsuits is crucial for success. The personal injury lawyers at the Nursing Home Law Center have the knowledge, experience, and dedication to handle wrongful death cases with the care they deserve.
Our experienced attorneys handle nursing home lawsuits on a contingency fee basis, which means if we don’t recover damages, you don’t owe us anything. If you’re ready to seek compensation for the wrongful death of your loved one,call (800) 926-7565 or fill out our form for your free consultation.