The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
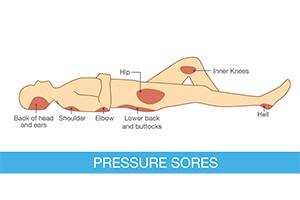
Pressure Ulcer Sites
Pressure ulcers, also known as bedsores, are common injuries for nursing home patients and those with limited mobility. They are caused by prolonged pressure on the skin, often on bony body parts with less padding. The constant pressure can lead to open wounds, which can become infected or cause death.
In this article, you’ll learn about common sites where pressure sores develop, the different stages, tips for preventing pressure ulcers, and your legal rights if you get them while receiving medical care.Pressure ulcers can indicate negligence, and Nursing Home Law Center can help you hold facilities accountable for your mistreatment.
Common Sites Pressure Sores Appear
Pressure sores, or decubitus ulcers, can appear anywhere on the body. However, several locations have a higher pressure ulcer risk. Areas with less fat and muscle protection can be common sites for a pressure injury because the bones are closer to the skin. They are more susceptible to shear forces and external pressure.
Sacrum and Coccyx
The sacrum and coccyx are among the most common areas in which pressure ulcers occur.
- Sacrum: A large bone located at the base of the spine. Sacrum bedsores will often develop on the buttocks above a patient’s tailbone.
- Coccyx: The coccyx is a small bone at the spine’s base. It’s also called the tailbone and attached to the sacrum. Coccyx bed sores develop in the middle of the buttocks.
These areas are highly susceptible to pressure ulcers, especially in bedridden individuals. Patients sit or lie down for prolonged periods, which can cause extended pressure. This can prevent wound healing.
Heels
Patients with limited mobility or who spend extended periods in bed can develop pressure ulcers on their heels. One of the most common causes is tight bedsheets. They can constrict a patient’s foot and ankle movement. Patients cannot move, causing a pressure injury to develop and preventing wound healing.
Hips and Ankles
Hips and ankles have bony protrusions that can lead to pressure ulceration, especially when patients lie on their sides. Because these extensions have little fat to cushion them, they are more susceptible to developing a pressure sore.
Elbows and Shoulders
Patients who spend a lot of time sitting in bed or in a wheelchair are at risk of developing pressure ulcers on their elbows and shoulders. This is especially true if the patient does not change positions regularly.
Elbow pressure ulcers can occur from resting your pressure points in the same spot for long periods. Shoulder bedsores occur when your shoulder blades constantly rub against a surface in the same position. The pressure on your shoulder blades causes a lack of blood flow to the area, leading to bedsores.
Back of the Head
Pressure injuries on the back of the head are common for those who are confined to bed, especially if a patient is paralyzed or in a coma. Head bedsores may not be immediately apparent because hair can hide them.
Ears
Ears can also be vulnerable to pressure ulcers. There are several reasons this pressure injury can develop, including:
- Friction from medical devices and oxygen tubing
- Pressure from constantly resting a patient’s head on the side
- Sleeping on your side
- Hearing aids, headphones, and other headgear
The lack of blood flow to the ears can lead to bedsores, and the constant friction prevents the wound from healing.

Stages of Pressure Ulcers

There are four stages of bedsores. Treating pressure ulcers can be more complex the more severe the injury. Higher-stage bedsores can cause life-threatening conditions and lead to death if left untreated.
Stage 1
Stage 1 pressure ulcers resemble bruises. Due to restricted blood flow, they appear as a warm red, blue, or purple area on the skin. Patients may report the skin burns or itches.
When you press the sore, it does not turn white. It will remain discolored no matter how much pressure you apply. The discoloration does not go away when you remove the pressure or reposition the body.
Stage 1 bedsores have unbroken skin. They are in the early stages, and proper wound care can prevent pressure ulcers from advancing to later stages.
Stage 2
Stage 2 pressure injuries have broken through the skin and can present as blisters, torn skin, or open wounds. They involve a partial-thickness skin loss, which is when a wound penetrates to the first skin layer (epidermis) or second skin layer (dermis).
Stage 2 pressure injuries can also be swollen and weeping. The skin around the bedsore will be discolored, and the area will be painful and warm. This fragile skin and underlying soft tissue have a greater risk of infectious complications without proper wound care.
Stage 3
Stage 3 chronic pressure ulcers extend deep into the skin, beyond the dermis and epidermis. It penetrates the subcutaneous tissue or deeper, which can cause severe health issues.
Stage 3 pressure injuries present like skin craters. Black tissue (eschar) or slough (discolored slimy tissue) in and around the wound can make it difficult to see inside it. The area can also be:
- Red
- Swollen
- Warm
- Filled with pus
- Leaking fluid
- Discolored around the edges
The area often smells foul, and the patient may experience fevers, chills, and high temperatures.
Stage 4
Stage 4 pressure injuries are the most severe. They often involve:
- Extensive tissue damage that extends beyond sot tissue
- Exposed bone, muscles, tendons, ligaments, joints
- Excruciating pain
- Blackened skin or yellow, gray, green, brown, or black pus
- Foul odor and drainage
Patients with stage 4 bedsores can face serious complications, including bone infection (osteomyelitis), septic arthritis, squamous cell carcinoma, or blood infection (sepsis). These can lead to organ damage, amputation, and even death.
They may need to receive skin grafts, remove dead tissue, and more to treat the wound. Topical treatment is usually not enough to heal stage 4 sores.
Unstageable
Advanced pressure injuries can be challenging to stage when eschar or slough obscures the wound bed. Medical professionals can cleanse the wound of dead tissue and determine the most effective treatment for unstageable pressure ulcers.

Pressure Ulcer Prevention Methods
Pressure injuries are avoidable, and there are several prevention methods that nursing homes can employto prevent them. A proper risk assessment will help caregivers develop a care plan to prevent bedsores.
Repositioning
Frequent repositioning is the best way to prevent bedsores, especially in those who cannot perceive pain. This can help relieve pressure on vulnerable areas, promoting increased blood flow to the site. It can also allow the skin to dry if moisture is present.
It is recommended that patients be repositioned every 15 minutes to prevent bedsores from developing. However, constant pressure reduction may not be possible in nursing homes, hospitals, and other treatment facilities because of understaffing. Failure to adjust the body position can lead to skin breakdown, soft tissue damage, and sores.
Skin Care
Proper skin care and hygiene can also reduce the risk of developing pressure injuries. The skin should be clean, dry, and moisturized to prevent friction. Additionally, nursing home staff should manage a patient’s incontinence, keeping the skin free of urine and feces.
A focus on skin wound care prevents shear due to friction during transport against bedsheets, wheelchairs, and more. Skin tears can quickly lead to injuries because of unrelieved pressure.
Support Surfaces
Specialized mattresses and cushions can help redistribute pressure throughout the body for at-risk patients. This will prevent friction on vulnerable bony areas, especially when patients are in bed for extended periods.
These pressure-reducing surfaces often help patients retain a 30-degree position, which is thought to prevent bedsores. Even if a patient is believed to be positioned at the ideal angle, they should still be frequently repositioned.
Nutrition and Hydration
Proper nutrition and hydration are essential for maintaining healthy skin and preventing pressure injuries.
- Balanced diet: Patients should get adequate nutrition and eat enough calories. Their diet should include a healthy mix of proteins, vitamins, and minerals. Vitamin C, copper, and zinc can help promote healing. If needed, meals can be taken orally or via a feeding tube and supplemented with multivitamins.
- Hydration: Patients should drink enough water each day to maintain skin elasticity. Some may need IVs to maintain proper hydration levels.
- Healthy weight: Patients who are underweight or overweight may have an increased risk of developing pressure injuries.
Your lifestyle can impact your risk factors for developing chronic wounds and how fast you can heal from them.

How a Nursing Home Injury Lawyer Can Help You
Pressure injuries are avoidable, and you have legal rights if you or your loved ones have experienced one due to nursing home neglect. Nursing home injury lawyers can help you get justice for your mistreatment. Here’s how.
Investigating Neglect
Your lawyer will investigate cases of pressure ulcers in nursing homes to determine if neglect occurred. They can review:
- Medical records: Your lawyer will secure comprehensive medical records, including a risk assessment, primary and secondary care reports, surgical records, and more, to determine if the nursing home’s lack of care caused your bedsores.
- Nursing home records: Many nursing homes have video surveillance, medical logs, and other documents to track treatment.
- Witness statements: Lawyers can interview doctors, nurses, care professionals, nursing home staff, other patients, and more to determine the environment and cause of your injuries.
They will gather evidence to build a case, including conducting an independent wound assessment if needed. They will use these records to prove the nursing home’s negligence led to your injuries.
Establishing Liability
Nursing home injury lawyers must prove negligence to hold the nursing home accountable for their actions. To prove neglect, your lawyer must establish the following.
- Duty of care: The nursing home had a duty of care to you or your loved one. The nursing home was obligated to care for them if they were a patient.
- Breach of care: The nursing home did not uphold its duty, leading to a breach of care. If a bedsore developed, they likely breached their care. The injury is preventable in most cases.
- Causation: The breach of care led to an injury. For bedsores, it’s likely the nursing home did not reposition you, keep you dry, or foster other circumstances that allowed a pressure ulcer to develop.
- Damages: You faced significant damages due to the pressure injury, including physical, emotional, or financial burdens.
Pressure injuries are preventable, and they can have life-threatening complications. Nursing homes should be liable for their actions, and lawyers can help you get compensation.
Seeking Compensation
Nursing home injury lawyers can help victims seek compensation for their injuries. You can recover the following compensation.
- Medical expenses: Doctor’s visits, physical therapy, surgeries, medication, ambulance rides, and other medical costs can be recovered.
- Emotional distress: Pressure injury victims can face severe emotional distress as a result of their injuries. They can develop depression, anxiety, and a loss of enjoyment of life.
- Pain and suffering: Pressure injuries can be excruciating. Patients can be awarded damages for their pain and suffering. This can be on a per-diem basis for their treatment or as a multiplier of their medical expenses.
Nursing home injury lawyers help you get the maximum compensation for your injuries. In some cases, you can recover punitive damages if the nursing home is found liable for gross negligence.
Lawyers understand how to navigate the legal system to get you the compensation you deserve.

Secure Expert Legal Representation!
Pressure ulcer injuries are preventable when nursing home patients are given the proper care and attention they are entitled to. If you suspect nursing home neglect, contact Nursing Home Law Center at (800) 926-7565 or complete the online contact form for a free consultation.
Our team of experienced bedsore attorneys can help you understand your legal options and provide recommendations to hold all liable parties accountable. You could receive compensation for your injuries.
Learn More About Bed Sores