The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
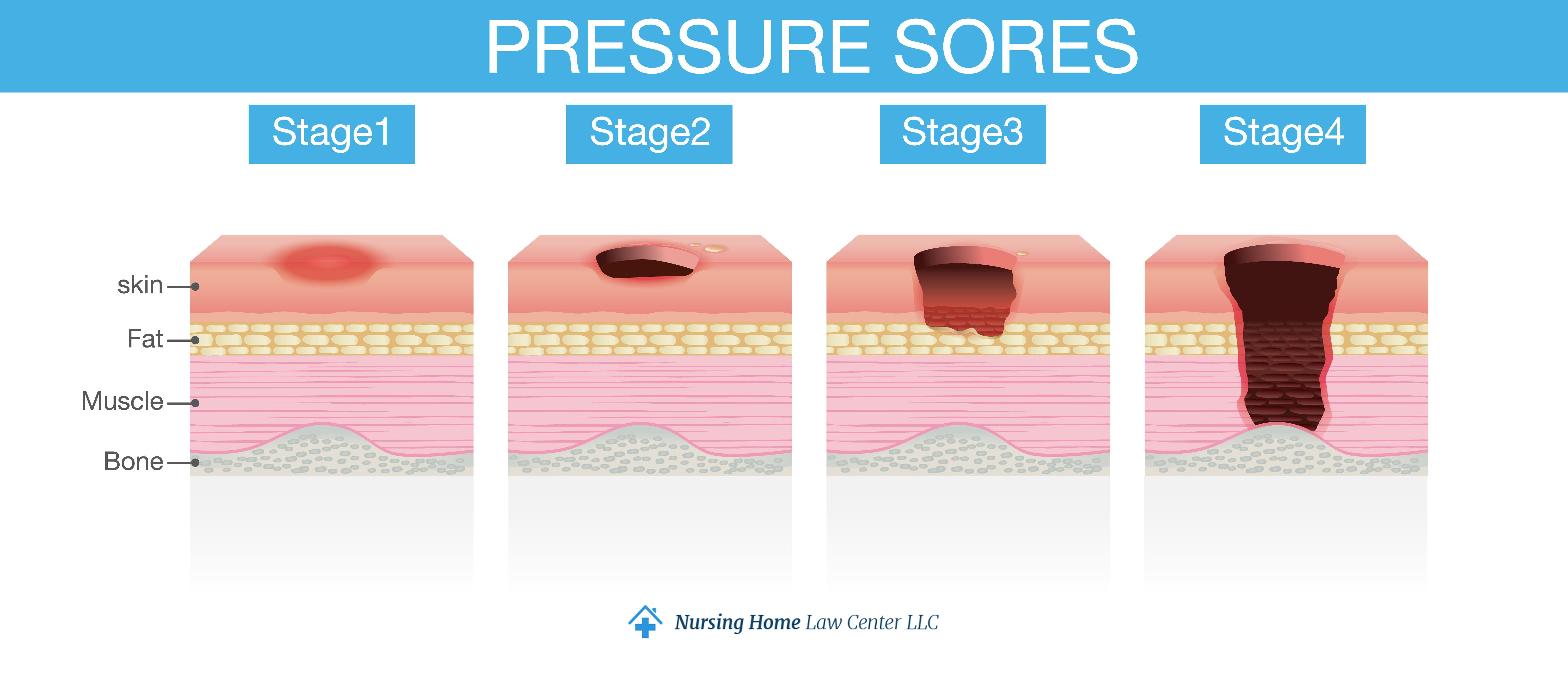
Stages of Pressure Ulcers
Pressure sores, or decubitus ulcers or bed sores, develop on the skin and the tissue underneath when an area of the body is exposed to prolonged pressure. As the pressure cuts off blood flow to the area, the tissue becomes deprived of oxygen, weakening and breaking down.
Pressure sores are common when people spend a long time in one position, and they can be highly painful, uncomfortable, and even life-threatening. We will discuss the four main stages of pressure ulcers and your legal options if they develop due to negligence.
Risk Factors for Pressure Ulcers
Certain health conditions and situations increase the risk of pressure injuries. Bedsores occur more frequently due to:
- Medical conditions – This includes diabetes, spinal cord injuries, heart disease, stroke, multiple sclerosis, and peripheral artery disease.
- Immobility – Prolonged bed rest or long periods of sitting in one position for too long decreases blood flow to areas under pressure.
- Poor nutrition – The lack of nutrients weakens the tissue and hinders healing, making patients more susceptible to a deep tissue injury.
- Incontinence – Moisture from urine or feces irritates the skin, posing a risk for inflammation and infection.
- Age – Older people are more vulnerable to pressure sores because their skin is more fragile.
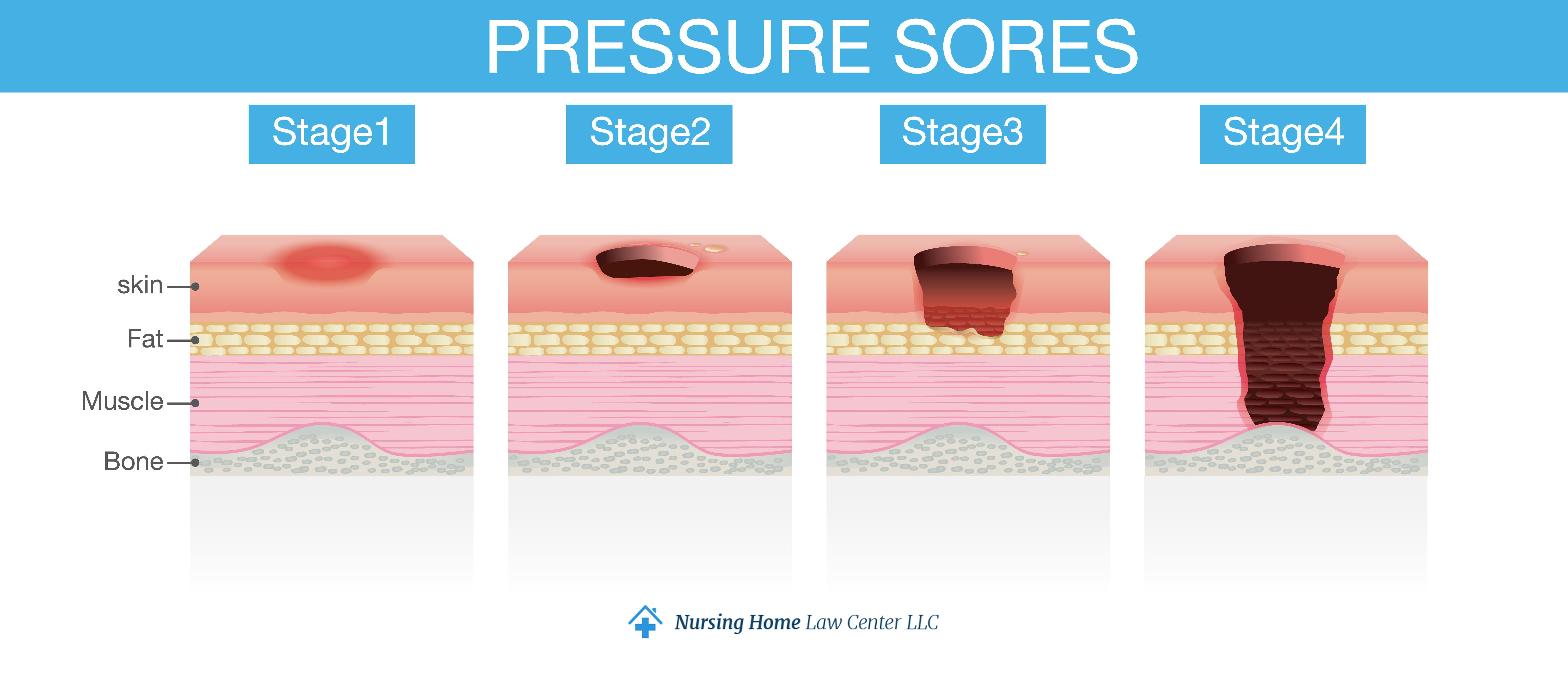
The Staging System for Pressure Ulcers
Health providers categorize pressure injuries into four stages, depending on the level of tissue damage. The pressure injury hasn’t broken through the skin or its second layer in the early stages. In the later stages, the wounds become deep.
There are also unstageable pressure sores, where necrotic tissue prevents immediate diagnosis, or a suspected deep tissue injury (SDTI), where the skin is intact, but deeper issues may be damaged underneath.
Stage 1
A stage one pressure injury appears as an area of persistent, non-blanchable redness on intact skin. This means the skin remains red even after you press it, unlike healthy skin, which turns white for a few seconds. A stage one pressure sore may feel warmer or cooler to the touch and may be itchy and painful.
This pressure sore may be more challenging for people with dark skin tones to notice it early on.
Stage 2
A stage two pressure ulcer is an open wound, as there is a visible break in the skin. It involves partial-thickness skin loss, affecting the epidermis and sometimes the dermis layer below. However, the deeper layers of skin and muscle are usually intact.
The wound often looks like a shallow open sore or fluid-filled blister in this stage. The wound bed (the exposed tissue) is usually pink or red.
Stage 3
Stage three decubitus ulcers are characterized by full-thickness skin loss, meaning the damage extends through the epidermis and dermis to the subcutaneous tissue. The subcutaneous tissue (the deepest layer of the skin) is damaged, and dead tissue may be present.
Sores at this stage look like deep, crater-like open wounds, with necrotic tissue appearing yellow or grayish. Tunneling or undermining of the wound is possible.
Stage three ulcers require immediate, aggressive treatment to remove dead tissue and heal the wound, as they’re at a higher risk for infection, including joint infections. Special bandages, such as foam dressings, are often used. A skin graft may be required.
Stage 4
The most severe pressure ulcers are stage four, characterized by full-thickness tissue loss that affects the muscle, tendon, or bone. Dead tissue may be present, appearing black or brown, and the wound edges might be undermined or have tunneling.
A stage four pressure ulcer can be large and deep, extremely painful, and swollen and inflamed in the surrounding area. Treating pressure sores at this stage may require surgical treatment. If the infection from the pressure sore spreads, it can affect the joints and bones and even lead to sepsis, septic shock, and death.
Preventing Pressure Ulcers
These classifications help physicians treat pressure sores and prevent them from getting worse. Prevention methods involve regularly monitoring and repositioning nursing home residents and providing them with proper nutrition, hydration, and skincare. Range of motion exercises can help prevent a pressure sore and promote healing by increasing blood circulation.
Regular Skin Inspections
Regular skin checks prevent pressure sores, especially in high-risk residents. Healthcare providers may even take photos of the sores to monitor wound healing and determine skin damage. This is also key for residents with darker skin color. Ulcers are most commonly found on:
- Shoulder blades
- Buttocks
- Coccyx
- Heels
- Bony areas
Pressure Relief Techniques
Nurses and other caretakers use various methods to relieve pressure, promote wound healing, and increase blood supply to the affected areas. These include:
- Repositioning – Changing the body position every couple of hours, depending on the pressure ulcer risk, to remove pressure.
- Cushions – Cushions, made of foam, gel, or inflatable materials, can be used in wheelchairs or seating areas to redistribute weight and reduce pressure on the skin.
- Special mattresses – These mattresses distribute weight evenly and periodically inflate and deflate different sections to improve circulation and minimize prolonged pressure.
Adequate Nutrition and Hydration
Proper nutrition and hydration prevent pressure wounds and promote healthy skin cells. A balanced diet rich in proteins, vitamins (A, C, and E), and minerals (like zinc) supports skin integrity and tissue repair.
Adequate calories and protein strengthen the body and help fight infection, while hydrated tissue becomes more flexible and less likely to break down.
Skin Care
Cleaning the skin surface with mild soaps, drying it gently, and moisturizing it can reduce the risk of damage. This is especially important for incontinent individuals who are at higher risk of developing severe sores.
Monitoring and caring for the skin makes it easier to notice signs of infection and include antibiotic therapy on time. This is crucial to catch signs of infection before the infection spreads.
Legal Implications of Pressure Ulcers
When someone you care about develops pressure sores due to a nursing home’s negligence, you can take legal action and possibly prevent this from happening to anyone else.
Negligence and Malpractice
Nursing homes have a duty of care to their residents, which includes providing wound care according to standards. When pressure sores develop or are left untreated, it may indicate that the healthcare provider failed to adhere to healthcare standards. This includes:
- Failure to implement care plans, change positions, perform skin inspections, and manage infections
- Understaffing
- Insufficient training
- Missing records of skincare, hygiene, and wound treatments
Liability of Nursing Homes
Due to their legal obligation to provide care, healthcare providers, hospitals, and nursing homes can face severe liability. A resident developing a decubitus ulcer may indicate negligence, particularly if the facility failed to follow established care protocols.
Nursing homes can face personal injury lawsuits from residents and their families, in which the families seek compensation for medical bills, rehabilitation costs, pain and suffering, and loss of quality of life.
Federal and state regulatory agencies may also punish the home through fines, sanctions, payment denials, and license suspensions.
Seeking Legal Advice
If you or a loved one has suffered from pressure injuries in a nursing home, it’s crucial to seek legal advice. These painful injuries can signal neglect or inadequate care, and you deserve to find justice for the highly uncomfortable, life-threatening experience.
An experienced attorney can help you navigate this difficult situation, gather the necessary evidence, and advocate for your loved one’s dignity and well-being. They can:
- Assess your case
- Gather evidence
- Consult medical experts
- Handle legal procedures
- Negotiate with insurance companies
- Represent you in trial, if needed

Secure Expert Legal Representation!
If you or a loved one experienced pressure ulcers in a nursing home, we advise you to seek legal help. An experienced nursing home attorney like those at Nursing Home Law Center can help you investigate the circumstances that led to pressure ulcer development and hold the facility accountable.
During a free consultation, we can help you understand your case, explain your rights, and advise you on available legal options.Finally, we work on a contingency fee basis. You can pay a percentage of your compensation if we win your case. Contact us today to schedule your free consultation.
Learn More About Bed Sores