The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
What Causes Bed Sores?
According to the Agency for Healthcare Research and Quality, more than 2.5 million Americans will develop bed sores annually. This condition disproportionately impacts the elderly and those with limited mobility because it is caused by restricted blood flow.
Read on to learn more about what causes pressure sores, risk factors, preventative measures, and how a nursing home injury lawyer can help you get justice if you develop pressure injuries while in care.
Nursing Home Law Center can provide legal representation when you are ready.
What are Bed Sores (Pressure Ulcers)?
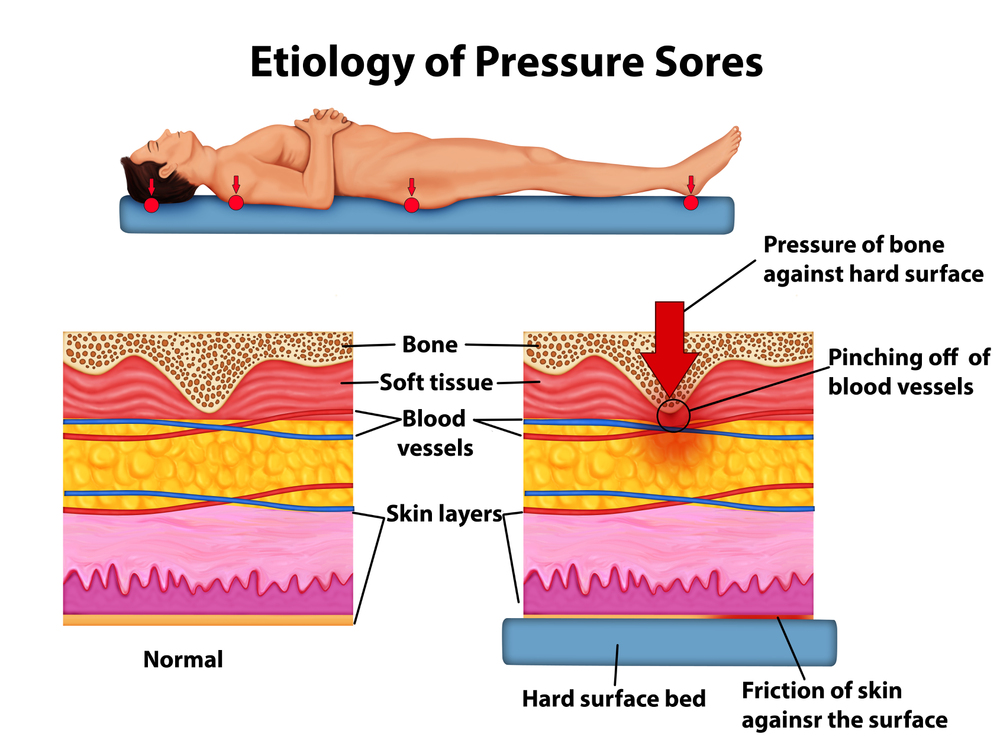
Bed sores, or pressure sores, occur when prolonged pressure is applied to the skin. This lowers blood flow and damages the skin, causing an underlying soft tissue injury. In severe cases, bones, joints, and muscles can be damaged as well. Depending on the stage, pressure-related sores can present like bruises or festering open wounds.
These sores can disproportionately impact elderly patients at nursing homes, as they have fragile skin and other conditions that can lead to these injuries. This ultimately causes them pain, depression, anxiety, and other mental health issues. In the most severe cases, these wounds can even be life-threatening.
How They Develop
Patients who are bedbound or limited to wheelchairs are often seated in the same position for prolonged periods. This causes extended pressure on the skin, leading to pressure wounds due to friction (which damages blood vessels), shear forces, skin tears, and more.
Examples of situations that can lead to pressure induced sores include:
- Sitting in bed without moving
- Being left in a wheelchair
- Friction from oxygen masks
- Lying on one side for an extended time
- Skin rubbing against tight clothing
- Laying on uneven surfaces for long periods of time
The longer the pressure is applied, the deeper the wound can get. In some cases, the affected limb may need to be amputated to stop the spread of infection.
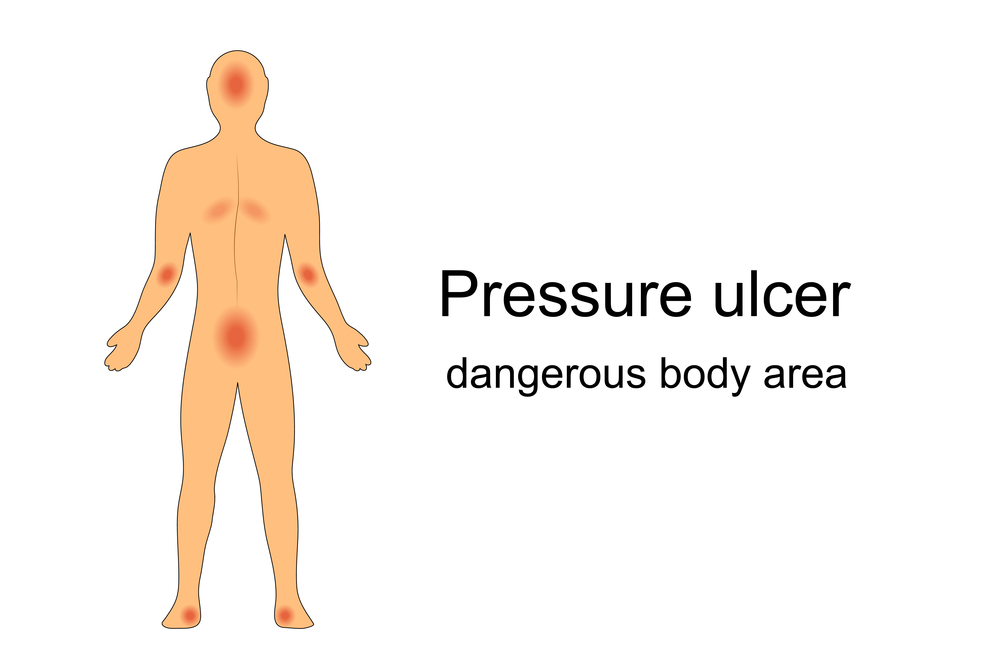
Where They’re Commonly Located
Bedsores can occur throughout the body but are most commonly present at bony areas with limited fat and muscle protection. This can include:
- Sacrum and coccyx
- Heels
- Hips
- Elbows
- Head
- Ears
- Shoulders
- Knees
The bony points of your body can more easily rub against surfaces, causing sores to develop.
Risk Factors for Pressure Ulcers
Nursing homes will do a risk assessment of a patient to determine if they’re likely to develop these injuries. Some of the risk factors include:
Immobility
Patients who have limited mobility or are completely bedridden have an increased risk of developing a sore. They cannot move their body without assistance, so they cannot change positions themselves.
Instead, they rely on nursing home staff to adjust their positioning in the bed or chair. This should happen every 15 minutes; however, understaffed nursing homes can cause some patients to go without moving for extended periods.
Poor Nutrition and Dehydration
Nursing home patients may be malnourished or dehydrated, which can cause their skin to lose elasticity and become damaged. This includes poor nutrition, like not eating enough calories or lacking the necessary nutrients to help their body heal. Additionally, dehydration can slow down essential body functions.
Incontinence
Patients suffering from incontinence can face a high risk of developing bedsores. Moisture from urine or feces can collect on the skin, making it easier to tear. These following situations can also lead to advanced stages of pressure-induced skin sores:
- Soiled adult diapers can cause friction when not changed frequently
- Soiled sheets can rub against the skin, leading to abrasions
Nursing home staff should keep the skin clean and change soiled linens to prevent infection and pressure-related skin sores.
Medical Conditions
Some other risk factors include medical conditions can increase a person’s likelihood of developing pressure-related skin injuries. These include:
- Diabetes: Some patients with diabetes have nerve damage, so they cannot feel discomfort. They may also have impaired wound healing.
- Obesity: Patients who are overweight may place more pressure on the body while lying in bed.
- Underweight: Patients who are too thin may have more bony protrusions on their bodies that can cause friction and lead to a pressure-related sore.
- Vascular conditions: Some vein conditions, including peripheral artery disease and chronic venous insufficiency, can impair a person’s ability to heal wounds.
- Dementia: Patients who suffer from dementia have less awareness of what’s going on around them. They may lose time and sit in the same position for too long.
- Cancer: Some treatments can reduce the skin’s strength and make it easier to develop bedsores. Left untreated, these sores, also known as, decubitus ulcers, can also cause cancer.
- Reduced sensation: People who have difficulty sensing pain and touch, such as those with spinal cord injuries, may not notice wounds forming. Without proper attention from caregivers or medical staff to relieve pressure, these wounds can worsen and lead to severe pressure-induced skin wounds and soft tissue injuries.
Any medical conditions that cause limited mobility or issues with blood vessels can lead to a high risk of developing pressure sores.
Age
Age can be another contributing factor to the development of pressure-induced skin injuries. Elderly patients often face the following issues.
- Limited mobility: Elderly patients often cannot move without aids or support.
- Skin health: They often have more fragile skin, making them prone to developing a sore.
- Health issues: Certain conditions can increase the risk of pressure sores.
Reduced blood flow and experiencing immobility for long periods of time can cause pressure-related sores in the elderly.
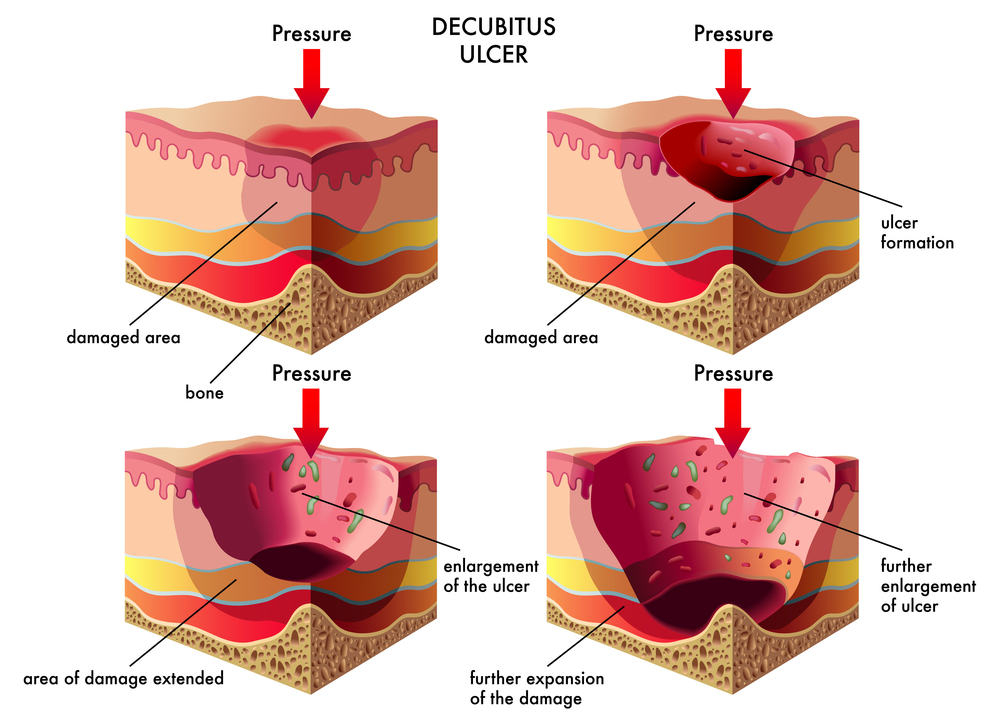
Stages of Pressure Ulcers
There are four stages of pressure sores, ranging from a mild inconvenience to a severe health concern.
- Stage 1: Stage one pressure injuries present like bruises. They may be patches of red, blue, or purple skin that do not blanch when applying pressure. They also do not fade when you relieve pressure. The skin is not broken in a stage one sore, but it can be hot and itchy for patients.
- Stage 2: Stage two pressure sores have broken the skin. They may look like blisters or simple cuts penetrating the dermis and epidermis skin layers. The deeper layers of skin around the sores are often discolored due to tissue damage or dead tissue, and the wound will be swollen and weeping pus or moisture.
- Stage 3: A stage three pressure sore is among the most serious. It has penetrated the subcutaneous tissue, causing crater-like wounds to develop. They are often red, swollen, filled with pus, and discolored. There may be black tissue present. This is dead skin.
- Stage 4: Stage four pressure injuries are the worst. The deep tissue pressure injury can extend to many areas of the body, including the bones, muscles, joints, ligaments, and tissues. They can even lead to bone infections. An untreated sore at this stage can sometimes develop into squamous cell carcinoma. The sore can also advance to the joint space and causes a joint infection, known as septic arthritis, posing a risk of severe joint damage and potentially leading to sepsis. This demands urgent medical treatment, as it can be life-threatening.
Sometimes, bed sores can be unstageable. Black tissue (eschar) or slough in various colors can block a healthcare professional’s view and prevent an accurate diagnosis. In these cases, doctors must cleanse the wound and remove any damaged or dead surrounding tissue so they can properly assess the injury.
Proving Nursing Home Negligence
Nursing home injury lawyers can help you prove negligence in your bed sore lawsuit. You will need to establish the following conditions.
Duty of Care
You must demonstrate the nursing home had a duty of care to you to prevent pressure ulcers. If you were a patient, you had a reasonable expectation of care.
Breach of Duty
Next, you must establish that the nursing home breached that duty by failing to provide appropriate care. This may include not moving a patient, resulting in decreased blood flow or lack of a wound healing plan. Any failure to prevent these pressure injuries from occurring should be investigated.
Causation and Damages
You and your lawyer must also prove that the breach caused harm, and this harm led the patient (or sometimes their families) to suffer significant physical, emotional, and financial damages. When you prove these conditions were met, you can hold the nursing home liable for negligence.
Signs of Neglect
Lawyers will look for the following conditions to help prove neglect. They include:
- Unsanitary conditions.
- Inadequate staffing
- Unsafe living conditions
- Patients left unattended for long periods of time
Increased reports of sores, injuries, and deaths can also be signs of neglect in nursing homes.
Preventing Pressure Sores
Nursing homes can easily avoid pressure-related sores if they adequately treat their patients.
Repositioning
Constant pressure reduces blood flow. However, frequent repositioning can promote blood flow to the skin and ease pressure on parts of the body with bony areas. It is recommended that patients change position every 15 minutes to stop pressure-related sores from developing or to let minor sores heal.
Skin Care
Proper skin care practices can prevent patients from developing pressure sores, including:
- Keeping the skin dry: Wet skin can easily lead to broken skin with friction.
- Washing the skin: Wash and sanitize the skin regularly to prevent bacteria from developing. Remove any urine or feces promptly.
- Properly moisturizing: Dry skin can catch and lead to skin damage and severe sores. Apply moisture barrier creams to maintain elasticity in the affected area of skin and the surrounding spots.
Support Surfaces
The ideal angle for a person to rest at is 30 degrees to prevent bedsores. Some specialized mattresses and cushions can help a patient maintain this position. It will redistribute the pressure on a person’s body, making it less likely to develop these sores.
Seeking Legal Help for Nursing Home Residents Suffering From Pressure Injuries
Lawyers can help victims of nursing home neglect get justice, including those who have developed pressure ulcers.
- Advocate: Lawyers will advocate for your rights, helping represent you throughout the legal process.
- Investigate: Lawyers gather evidence to build a solid case to help you recover compensation.
- Negotiate: Lawyers negotiate with nursing homes and insurance companies to help you reach a fair settlement. If an agreement can’t be reached, they represent you in court.
Lawyers can help hold nursing homes accountable for their actions and prevent these conditions from occurring again.
Compensation for Damages
Victims can recover various types of compensation for their injuries, including:
- Medical expenses: Doctor’s visits, surgery, hospitalization, physical therapy, and costs of medication, can be recovered.
- Emotional distress: Many victims can face mental health issues, including depression and anxiety, as a result of their injuries.
- Pain and suffering: Bedsore victims can receive compensation for their physical pain and suffering.
- Punitive damages: Victims can also recover punitive damages if a nursing home is found guilty of gross negligence. These are intended to punish the nursing home and deter them from maintaining these conditions.
How much compensation you can recover depends on your case, and a nursing home lawyer can help you understand your legal options.
Secure Expert Legal Representation!
Pressure-related sores are preventable, but if they occur, it can be a good indication of nursing home neglect. If you or your loved one are a victim of pressure injuries, contact the Nursing Home Law Center for a free consultation.
Our team can explore the details of your case and recommend an appropriate legal course of action. Call us at (800) 926-7565 to get started.
Learn More About Bed Sores