legal resources necessary to hold negligent facilities accountable.
Naperville Nursing Home Abuse Lawyer
 Nursing home abuse and neglect is a serious but often hidden problem in the United States. Statistics show that elderly people residing in nursing facilities are at risk of becoming victims of potential harm or injury at the hands of their caregivers or other nursing home patients. While physical abuse is the most obvious, emotional and mental abuse are less obvious but more common.
Nursing home abuse and neglect is a serious but often hidden problem in the United States. Statistics show that elderly people residing in nursing facilities are at risk of becoming victims of potential harm or injury at the hands of their caregivers or other nursing home patients. While physical abuse is the most obvious, emotional and mental abuse are less obvious but more common.
Our Naperville, Illinois, nursing home abuse lawyers at Nursing Home Law Center, LLC have handled many personal injury cases of elder abuse, neglect, and mistreatment and have seen a significant rise in the incidence of nursing home negligence in Naperville and throughout Illinois.
Any time abuse takes place in a caregiving facility, families who entrusted the care of their aging parents to these nursing homes, feel justifiably angry. Was your loved one injured or did they die unexpectedly from neglect while living in a Naperville nursing home? Let the affiliate Illinois personal injury attorneys at Nursing Home Law Center protect the rights of your family.
Contact the Naperville nursing home abuse lawyers at (800) 926-7565 (toll-free phone number) today to schedule a free consultation to discuss filing a claim for compensation. All confidential or sensitive information you share with our legal team remains private through an attorney-client relationship.
Nursing Home Abuse: A Serious Issue With Devastating ConsequencesDealing with the aging process is difficult for disabled and elderly individuals and their loved ones. Unfortunately, it's all too common and many cases go unreported, leaving the victim feeling frightened or alone in their struggle of mistreatment at the hands of those whom they trusted to provide care or live among in the facility.
Many cases go unreported - leaving those who are suffering from mistreatment even more vulnerable than before they were placed into nursing homes.
US Nursing Home Abuse StatisticsNursing homes can be a good option for some elderly or disabled loved ones needing around-the-clock care that cannot be provided by family members. However, many nursing home residents suffer abuse and neglect which is why it's important to investigate your options before putting someone in this type of facility
National Center on Elder Abuse research shows ten percent (10%)of people staying in nursing facilities at intervals receive abusive treatment. About seventeen percent (17%) of long-term nursing home residents experience mistreatment spanning from minor to severe according to the National Center on Elder Abuse.
As referenced by the World Health Organization (WHO), elder abuse is a "single or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person".
Illinois/Naperville Nursing Home Abuse StatsIn Illinois, it is estimated that one in six nursing home patients receiving long-term care experiences abuse each year.
The Illinois Department of Public Health (IDPH) is responsible for investigating all complaints related to abuse, mistreatment, and neglect in nursing facilities
In 2018, the IDPH substantiated 2,241 complaints of physical assault, sexual abuse, emotional abuse, financial exploitation, and gross neglect in Illinois nursing homes.
Of the substantiated complaints:- Forty percent (40%) were associated with physical assault
- Twenty-nine percent (29%) were attributed to emotional abuse
- Twenty-two percent (22%) involved financial exploitation
- Seven percent (7%) were cases of sexual abuse, and two percent (2%) were related to gross neglect
Elder abuse is a serious problem in the United States and, unfortunately, it is only getting worse as the baby boomer population continues to age. Nursing home abuse can have devastating consequences for victims, both physically and emotionally.
Types of Nursing Home Abuse and NeglectThere are many different types of nursing home abuse, mistreatment, and neglect that leave injured victims devastated, including:
- Physical abuse could involve hitting, slapping, poking, or kicking a resident. The most serious form of physical harm is when patients are beaten so badly that it causes bruises and swelling on their bodies which might lead to other health complications.
- Emotional abuse includes name-calling, belittling, mocking, or otherwise verbally assaulting a nursing home resident. This type of abuse can also involve isolating a patient from other residents or visitors as a way to control them.
- Sexual abuse is any sexual interaction between a nursing home resident and another without the resident's consent. An alleged sexual assault could involve a staff member, visitor, family member, employee, vendor, or another resident. This form of horrific abuse might include rape, molestation, or any unwanted touching of the resident's genitals or other private areas.
- Financial exploitation could be a nursing home employee, visitor, family member, or other who takes advantage of a resident's financial situation for personal gain. Financial abuse might involve anything from stealing money out of the resident's account, taking personal belongings, or using the resident's credit card without permission.
- Gross neglect involves a nursing home staff member failing to provide the basic needs of a resident, such as food, water, or medical care. This type of neglect can quickly lead to serious injury or death.
- Pressure Sores (bed sores) are some of the most common signs of nursing home abuse or neglect. These painful wounds form when a person is left in the same position for too long without being moved. While they can occur anywhere on the body, they are most likely to form on bony areas, such as the hips, tailbone, back, or heels.
Do you suspect that your loved one is the victim of nursing home abuse or neglect? Act now to prevent further harm and get your loved one the help they need.
Nursing Home Abuse, Mistreatment and Neglect: Common CausesNursing homes have often been seen as a safe haven for senior citizens who need assistance with daily living tasks. However, nursing staff members and residents alike can be victims of abuse in these facilities that go unnoticed or unpunished due to poor reporting procedures by facility owners.
Nursing Home Abuse Are Tragic Realities That Can Be Prevented!Identifying neglect and abuse at the facility can help protect yourself or your loved one from becoming a victim. Some of the most common causes of abuse and neglect include:
- Lack of staff training and supervision: Often, nursing homes are understaffed and do not have the proper resources to provide adequate care for all of their residents, leading to a lack of individualized attention and an increased risk of abuse or neglect.
- Poor communication between staff members: Could lead to a breakdown in the quality of care that is provided. This preventable problem can be especially dangerous for residents with special needs who require around-the-clock care.
- Lack of security : Nursing homes should have security measures in place to protect residents from potential abusers. However, many facilities do not have adequate security, which can leave residents vulnerable to attack.
- Residents not being treated with dignity or respect: Being disrespected could lead to a feeling of powerlessness and isolation among residents, which can increase the risk of abuse or neglect.
- Staff members who are overworked or underpaid: Could lead to a feeling of frustration and resentment, which can be taken out on the residents.
- Poor environmental conditions: Such as insufficient lighting or heating could expose residents to dangerous hazards or health risks.
These are just some of the common causes of nursing home abuse, mistreatment, and neglect. If you suspect that your loved one is the victim of any type of abuse or neglect, it is important to act quickly to get them the help they need.
The Most Vulnerable Nursing Home Residents With High Risk of Abuse or NeglectAbuse and neglected nursing home residents are often scared to speak up, especially if they are elderly or disabled. These individuals are often unable to care for themselves and rely on staff members to meet their needs. Those most at risk could include:
- Elderly patients with dementia or Alzheimer's disease: These individuals may be unable to communicate what is happening to them or may not be able to remember incidents of abuse.
- The physically frail, or those without an assigned social worker: These residents are often unable to fight back or defend themselves if they are being abused.
- Individuals who have a history of abuse or neglect: These individuals may be more likely to be targeted by abusers because they are seen as easy targets.
- Nursing home residents who are isolated from family and friends: These residents may be more likely to be abused or neglected because they have no one to speak up for them.
- Individuals with physical disabilities: Residents who are bedridden or have difficulty moving around are at a higher risk of being abused or neglected due to their lack of mobility.
- Residents who are non-verbal: These residents may have difficulty communicating their needs or may be unable to speak up if they are being abused.
Providing substandard care can lead to life-threatening medical conditions, including urinary tract infections, influenza, pneumonia, gastrointestinal infections, and soft tissue infections.
Preventing Nursing Home Neglect and Abuse: What to Do to Protect a Loved OneNursing home residents often feel powerless when it comes to protecting themselves or another person in their life. However, there are steps that everyone has power over how they live out the last days on earth because of this issue - being proactive will help prevent any harm coming your way.
With enough knowledge about what constitutes normal behavior for nurses and certified nursing assistants at elderly care facilities (and whether something seems right), we all have control over whether our family member(s) receive optimal treatment.
The following are some things you can do to prevent nursing home abuse and neglect:
- Research nursing homes in your area: When you are looking for a nursing home for your loved one, be sure to do your research. Read online reviews and speak to other families who have had experience with nursing homes in your area.
- Tour the facility: Once you have narrowed down your choices, schedule a tour of the facility. Walking around the environment and meeting the staff can identify immediately apparent problems.
- Ask questions: When you are touring the facility, be sure to ask the staff questions about their policies and procedures. It will help you to get a better understanding of how the facility is run.
- Speak up: If you have any concerns about the care your loved one is receiving, be sure to speak up. You should also report any suspicions of abuse or neglect to the proper authorities.
- Stay involved: One of the best ways to prevent abuse or neglect is to stay involved in your loved one's life. Be sure to visit often and stay in touch with the staff.
Protect your loved one by understanding the common signs of abuse and neglect, including:
- Bruises, welts, or burns that are not consistent with the explanation given
- Broken bones or fractures
- Unexplained cuts or lacerations
- Signs of restraint, such as marks on the wrists or ankles
- Sudden weight loss or gain
- Changes in mood or behavior, such as withdrawal from social activities
- Development of bed sores
- Unkept appearance
- Positive STD tests
- Unsanitary living conditions, such as soiled bedding or a lack of personal hygiene
Have you noticed any of these signs? Speak up and talk with the facility administrator. You should also report your concerns to the proper authorities including Adult Protective Services and the police.
Discuss your legal issues with our abuse and neglect lawyers. Our Naperville, IL legal team can help you seek justice and receive a fair settlement if your loved one (victim) suffered needlessly through someone else’s negligence, mistreatment, or abuse.
What to Do if You Suspect Nursing Home Abuse or NeglectIf you suspect that your loved one is the victim of nursing home abuse or neglect, there are a few steps that you can take to help them:
- File a formal complaint with the facility administrator, who by law must investigate the allegations.
- Report the abuse or neglect to the proper authorities including Illinois Adult Protective Services, the police, or the Department of Health and Human Services.
- Get in touch with Naperville nursing home abuse lawyers to discuss your legal options and file a lawsuit if necessary.
- Move your loved one to a safe environment where they can receive the care and attention that they need.
Act now to protect your loved one from further harm. Nursing home abuse, mistreatment, and neglect are serious problems that can have devastating consequences.
Acting now can help ensure that your loved one gets the justice and compensation they deserve.
Relocating an Abused or Neglected Loved One into Another Nursing HomeFinding the right nursing home for a loved one is a daunting task when searching for a facility that will provide the best possible care. Families relocating a disabled, rehabilitating, or elderly loved one abused or neglected in their existing nursing residence must ensure they are placed somewhere that will ensure they are protected.
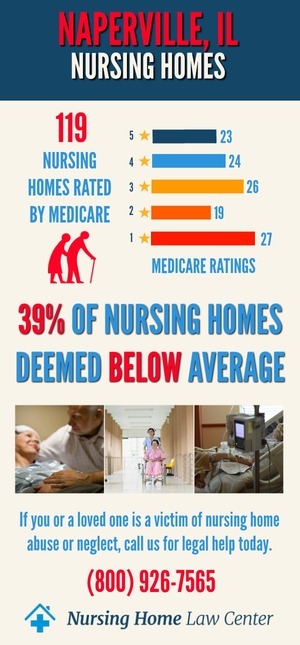
Medicare.gov maintains a database with continually updated information on all nursing facilities in the community. The information identifies all problems, investigations, complaints, and violations of the nursing home.
Things to consider before relocating a loved one into a new nursing home residence include:
- The nursing home licensing status
- The specific type of abuse or neglect that occurred
- The results of any investigations by the state or local authorities
- Whether there are pending lawsuits against the facility
- The overall rating of the nursing home on Medicare.gov
Take your time when making a decision about where to relocate your loved one. Research all available options to ensure you are making the best decision for their safety and well-being.
Visit the Nursing Facility FirstYour research must include visiting the nursing facility and meeting the nursing staff and administrator. Taking a tour of the facility can help you identify any potential safety concerns and get a feel for the overall atmosphere.
Make sure to ask plenty of questions about the facility, its policies, and procedures. Some important questions to ask include:
- How do you handle complaints or concerns from residents or families?
- What is your policy on resident restraint?
- How do you prevent the spread of infection?
- What is your nurse-to-residents ratio?
- What are your policies on medication administration?
- What type of training do your staff members receive?
Once you have gathered all the information, take some time to think about your decision. If you have any doubts, it is always best to err on the side of caution and choose another facility.
Preventable Bed Sores: Life-threatening Health ConcernsThe Centers for Medicare and Medicaid Services (CMS) reports any developing bed sore (pressure sore, pressure wound, pressure ulcer, decubitus ulcer) as a "never event." The agency claims that nearly all pressure wounds are preventable at any stage when doctors, wound care specialists, and the nursing staff follows skin care protocols.
Most bed sores develop in a hospital setting or nursing home environment due to:
- Malnutrition and dehydration: When a person does not receive the proper nutrients, their skin becomes thin and frail, making it more susceptible to injury.
- Lack of mobility: When a person is confined to a bed or wheelchair, they are at an increased risk for developing pressure sores.
- Incontinence: When a person is incontinent, their skin is constantly exposed to urine and feces, which can lead to the development of bed sores.
- Shear and friction movement: When a person is moved frequently, their skin can rub against the sheets or clothing, which can cause bed sores.
Bed sores are painful and can lead to a number of serious health complications, including:
- Infection: When bed sores become infected, they can become life-threatening. The infection can spread to the bloodstream and throughout the body.
- Sepsis: A potentially life-threatening condition that occurs when an infection spreads through the bloodstream.
- Cellulitis: A bacterial skin infection that can spread quickly and become life-threatening.
- Gangrene: A serious condition that occurs when the blood supply to an area of the body is cut off. It can lead to the death of tissue and, in some cases, amputation.
There are a number of steps that can be taken to prevent bed sores, including:
- Keeping the skin clean and dry: Washing the skin with a mild soap and water and drying it thoroughly.
- Avoiding friction and shear: Avoiding it can be done by using special mattresses and bedding that reduce friction and shear.
- Positioning the body: Turning and repositioning the body every two hours to avoid putting pressure on one area for too long.
- Providing nutrition and hydration: Making sure the person is getting enough fluids and nutrients.
The number of deaths each year in the United States caused by elderly abuse is difficult to determine because elder violence often goes unreported.
However, an NIA (National Institute on Aging) study and NCIPC (National Center for Injury Prevention and Control) report found that approximately 1,600 nursing home residents die annually as a result of physical or sexual abuse.
Losing a loved one is always challenging, but when they die as the result of abusive or neglectful behavior in a place that was in charge to protect them, it is heartbreaking.
Families can file a nursing home abuse case involving wrongful death to recover financial compensation when their loved one died of negligence or abuse at the facility. Qualifying family members could include a surviving spouse, child, grandchild, or other dependents.
Nursing home abuse claims that are successfully resolved through a negotiated settlement or jury award should provide compensation to pay for:
- Funeral and burial costs
- Medical bills related to the decedent’s injuries or illness
- Loss of earnings and benefits
- Pain and suffering
- Mental anguish
- Punitive damages (in some cases)
The first thing that families should do when they suspect mistreatment is to contact an experienced Naperville nursing home abuse lawyers who handle these types of cases.
Proving a Case for Wrongful Death in a Nursing Home SettingTo prove a case for wrongful death against a nursing home, the following must be established:
- The nursing home and staff members (defendants) owed your loved one a duty of care
- The defendants breached their duty of care
- Your loved one died as a result of the breach (causation)
- You (the plaintiff) have suffered damages as a result of your loved one’s death that can be proven in court
Resolving a compensation case takes time and a comprehensive understanding of Illinois civil tort laws. Typically, victims will hire a personal injury lawyer specializing in nursing home abuse/neglect cases.
Our Naperville nursing home abuse lawyers will work with you to investigate the circumstances surrounding your loved one’s death, gather evidence, interview witnesses, and file all the necessary paperwork in court.
Should the nursing home abuse case goes to trial, your Naperville, IL, personal injury lawyer will also represent you in front of a judge and jury, present evidence and hire professional experts to provide testimony to hold the defendants accountable.
Most nursing home abuse and neglect cases are resolved through settlement negotiations between the victim’s personal injury lawyer and the nursing home’s insurance company.
In some cases, though, a trial may be necessary to get the full amount of compensation that you deserve. If this happens, your Naperville nursing home abuse lawyers will be with you every step of the way to ensure that your rights are protected.
Speak to Naperville Nursing Home Abuse Lawyers About Your Personal Injury CaseThe Naperville nursing home abuse lawyers at Nursing Home Law Center have represented many victims of nursing home neglect and abuse in Illinois. Our team of dedicated and knowledgeable nursing home abuse lawyers currently provides legal representation in cases involving neglect and abuse occurring in nursing facilities in
- Kane County
- Dupage County
- Cook County
- Lake County
Contact our affiliate Naperville nursing home abuse lawyers today at (800) 926-7565 or use an online contact form. You can schedule a free consultation to speak with one of our skilled personal injury attorneys for a free case review.
Our personal injury law firms handle all cases of abuse, neglect, and mistreatment through contingency fee agreements. It means we are only paid for our legal services after obtaining an award for you in court or negotiating an out-of-court settlement on your behalf.
Resources: DuPage County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
DuPage County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
