legal resources necessary to hold negligent facilities accountable.
Champaign Nursing Home Abuse Lawyer
 Nursing home residents face a heightened risk of abuse, which can lead to serious physical injuries, psychological trauma, and, in some cases, death. This abuse often goes unreported, leaving the victims to suffer in silence.
Nursing home residents face a heightened risk of abuse, which can lead to serious physical injuries, psychological trauma, and, in some cases, death. This abuse often goes unreported, leaving the victims to suffer in silence.
Our nursing home abuse attorneys at Nursing Home Law Center, LLC are skilled in uncovering and addressing these hidden cases of abuse. We advocate for the victims, seeking justice and compensation to aid their recovery and protection.
Understanding Nursing Home AbuseIn Champaign, Illinois, nursing home abuse is a serious issue that often goes unnoticed and unreported. Understanding what constitutes abuse is the first step towards combating this injustice. As experienced nursing home abuse lawyers, we are committed to shedding light on this critical issue, ensurfging from physical to emotional harm inflicted on vulnerable elderly residents. It is a violation of trust and a legal offense that demands immediate attention. Recognizing and addressing nursing home abuse and assisted living facilities is essential to safeguard the well-being of our senior citizens.
The Need for Legal RepresentationSeeking legal representation is crucial in cases of nursing home abuse. A qualified Illinois nursing home abuse lawyer can provide the necessary guidance and support to navigate the complex legal landscape. We understand the intricacies of these cases and are dedicated to ensuring that justice is served for the abused and neglected.
Types of Cases HandledOur Champaign elder caregiving home law firm handles various types of nursing home abuse cases, such as:
- Physical abuse
- Sexual abuse
- Financial abuse
- Emotional abuse
- Negligence and medical malpractice
- Wrongful death
Each type of mistreatment case presents unique challenges and requires a specialized approach. Our team of nursing home abuse attorneys is equipped with the knowledge and experience to tackle these diverse cases effectively.
Recognizing Forms of AbuseCommon signs of mistreatment include sudden changes in behavior, unexplained injuries, and unusual financial transactions. Recognizing these indicators is the first step in protecting residents from further harm.
Identifying the different forms of abuse in nursing homes is critical for taking timely action. As Champaign nursing abuse attorneys, we emphasize the importance of awareness among family members and staff members to ensure the safety of all residents.
Physical AbusePhysical abuse in nursing homes can manifest as unexplained injuries, such as bruises,broken bones, or cuts. It's crucial to recognize these signs, report any suspicions of abuse to authorities, and seek legal help.
Emotional AbuseEmotional abuse, though less visible, can be equally damaging. Signs include:
- Sudden changes in behavior
- Withdrawal
- Fear among elderly residents
This form of abuse requires immediate attention to prevent long-term psychological harm.
Financial AbuseFinancial exploitation involves the unauthorized use of an elderly person's finances or assets. It's essential to monitor financial transactions and changes in wills or power of attorney, especially if the elderly resident is not fully aware or consenting.
Sexual AbuseSexual abuse in nursing homes is an alarming violation that often goes unreported. Recognizing and addressing any signs of non-consensual sexual contact is crucial for the safety and dignity of residents.
NegligencePatients can get severely injured when the nursing home staff fails to follow protocols to provide adequate care. Negligence can occur through the following:
- Medical malpractice
- Failure to provide appropriate medical care
- Facility-acquired pressure sores
- Medication errors
According to the National Center on Elderly Abuse, nursing home abuse is more prevalent than most people realize. This underreported issue affects numerous elderly patients, causing both physical and emotional damage. Understanding the extent of this problem is crucial for implementing effective preventative measures.
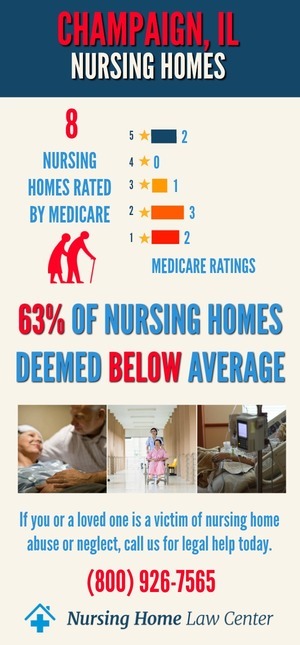
Nursing Home Statistics in Champaign, IllinoisData on the frequency and types of elder abuse in nursing homes reveal a disturbing trend. These statistics highlight the need for increased awareness and more robust protective measures for elderly victims in nursing facilities.
Centers for Medicare and Medicaid Services (CMS) RatingsIn December 2023, the CMS evaluated nursing homes in Champaign, Illinois, to assess their overall quality of care and services. The findings revealed a concerning situation where all ten facilities assessed, constituting a staggering 90%, received ratings categorized as "below average" or "much below average" by CMS.
Facilities Cited for Nursing Home AbuseAmong these nursing homes with below-average ratings, some were further scrutinized by inspectors for instances of abuse and neglect. It is vital to bring attention to these facilities to ensure resident safety. The following Champaign, Illinois, nursing homes were identified as having received citations for abuse:
- Accolade Healthcare of Savoy
- Goldwater Care Gibson City
- Piatt County Nursing Home
The prevalence of below-average ratings and instances of abuse highlights the urgency of addressing these issues to protect the vulnerable residents in these facilities.
Seeking Justice and AccountabilityAchieving justice and accountability for victims of nursing home abuse is a primary goal of our Champaign nursing home lawyers. We are dedicated to representing the interests of the abused and their family members, ensuring that they receive the compensation and justice they deserve.
Legal Support and RepresentationOur legal team offers comprehensive support and representation in nursing home abuse cases. We help victims navigate the legal process, from filing lawsuits to representing them in court. Our commitment is to seek compensation and justice and hold responsible parties accountable for their actions.
Protecting Your Loved One in a Nursing or Assisted Living FacilityProtecting your loved ones in caregiving homes is of utmost importance. It involves being vigilant about their care and well-being and taking immediate action if signs of abuse or neglect are observed.
Steps to Take in Nursing Home Abuse ClaimsIf you suspect abuse in a nursing home, it is vital to take action immediately. This includes:
- Documenting signs of abuse
- Reporting to the appropriate authorities, including the following:
- Department of Human Services' OIG Hotline
- Senior HelpLine at (800) 252-8966 or (888) 206-1327 (TTY).
- Illinois Department of Public Health
- Seeking legal advice
Early intervention can prevent further harm and ensure the safety of your loved one.
Get Legal Help NowIf you or a loved one has been a victim of nursing home abuse in Champaign, it is crucial to seek legal help immediately. Our Champaign nursing abuse attorneys are here to offer guidance and support throughout the entire legal process.
Contact our law firm for a free consultation or to learn more about how we can assist you. Our dedicated nursing home lawyers are ready to help you seek justice and compensation for the wrongs suffered.
Hiring Our Nursing Home Law Center to Defend Your Family's RightsChoosing the proper legal representation is crucial in nursing home abuse cases. Our Champaign nursing home lawyers at the Nursing Home Law Center, LLC, are committed to defending the rights of your family and loved ones. We bring expertise, compassion, and a relentless pursuit of justice to every case we handle.
Our top priority is ensuring that nursing facilities are held accountable for their actions. Our nursing home neglect lawyers work tirelessly to represent clients effectively, seeking compensation for the harm caused and advocating for improved standards of care in nursing homes.
Trust us to be your voice and fight for the rights and dignity of your loved ones. Contact a nursing home abuse attorney immediately at (800) 926-7565 to schedule a free case evaluation. We accept all cases on a contingency fee arrangement, meaning you only pay our fees once we resolve your case.
 Champaign County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Champaign County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
