legal resources necessary to hold negligent facilities accountable.
Tucson Nursing Home Abuse Lawyer
 The neglect of nursing home residents often results in critical medical conditions being overlooked, leading to a decline in health and well-being. This form of negligence can manifest in bedsores, malnutrition, or inadequate medical treatment, exacerbating existing health issues.
The neglect of nursing home residents often results in critical medical conditions being overlooked, leading to a decline in health and well-being. This form of negligence can manifest in bedsores, malnutrition, or inadequate medical treatment, exacerbating existing health issues.
The team of nursing home abuse attorneys at Nursing Home Law Center, LLC focuses on these neglect cases. We strive to secure the necessary medical care and compensation received for affected residents and their families.
The Prevalence of Nursing Facility AbuseNursing facility abuse in Tucson, like many other places, is a grave concern that affects numerous vulnerable individuals. This issue is not isolated; it's a nationwide problem with profound implications for the elderly and their families.
Understanding the prevalence and severity of nursing facility abuse is vital for implementing effective preventative measures and providing appropriate support to victims.
Nationwide ConcernsElder abuse is a significant issue across the United States, affecting thousands of elderly residents in various care facilities. Reports and studies indicate that abuse in nursing homes is far more common than most people realize, often going unreported due to the vulnerability of the victims and the hidden nature of the abuse.
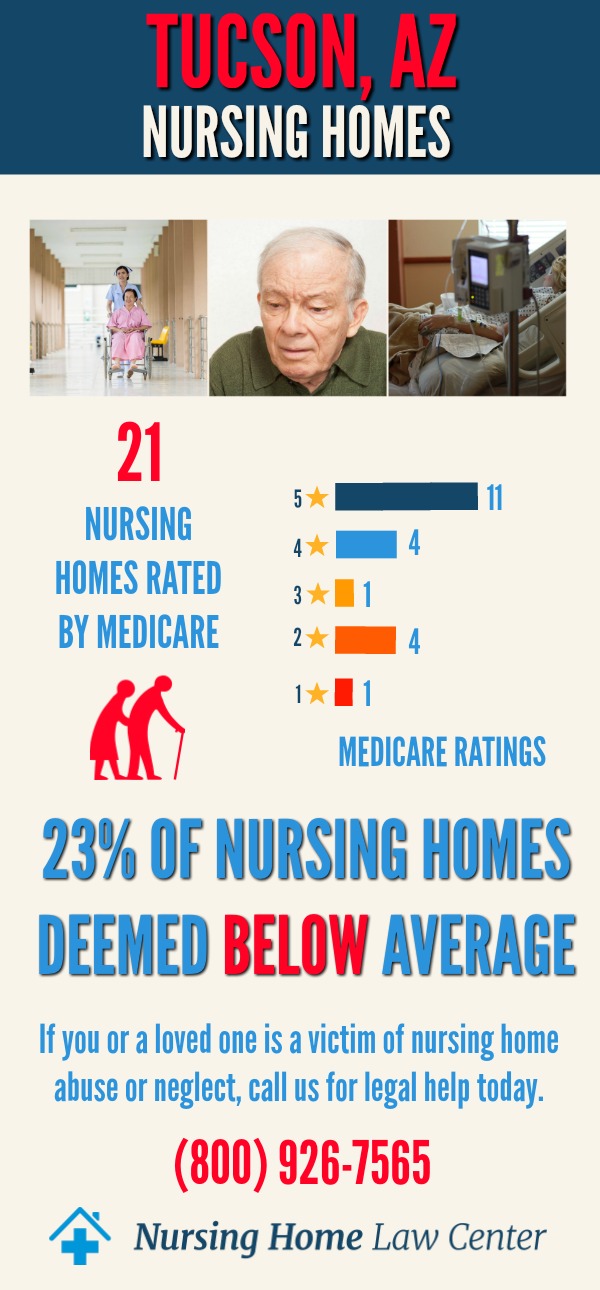
Tucson, Arizona Nursing Home StatisticsIn December 2023, the Centers for Medicare and Medicaid Services (CMS) conducted comprehensive evaluations and ratings for nursing homes in Tucson, Arizona. These ratings are invaluable tools for families seeking the best care for their loved ones. Unfortunately, the data reveals a troubling trend, with many area nursing homes falling below the expected standards of care.
Alarming FindingsBased on CMS data, out of the 25 nursing homes assessed in Tucson, a concerning 12 facilities, representing nearly half of them at 49%, received ratings of "below average" or "much below average." These ratings cause alarm and prompt serious questions about the quality of care provided in these nursing homes.
Among the nursing facilities with unfavorable ratings, one facility stands out due to inspectors citing Pueblo Springs Rehabilitation Center for instances of abuse.
Families entrust these facilities to provide proper care for their elderly family members, but sometimes, that trust is broken. Families and individuals must be aware of their legal rights and options when they suspect or encounter abusive behavior or substandard care.
The Different Forms of Nursing Home Neglect and AbuseNeglect and abuse encompass a range of harmful behaviors that adversely affect residents. Different forms of abuse have unique characteristics and impacts, making it crucial to understand these distinctions for proper identification and intervention.
Types of Abuse and NeglectThe abusive or negligent actions within care home facilities and assisted living facilities can inflict significant harm on vulnerable residents.
- Physical Abuse in care homes involves the use of force that causes physical harm to residents. This can manifest as hitting, slapping, pushing, or other forms of physical violence, resulting in injuries such as broken bones, unexplained bruises, or other serious injuries.
- Sexual abuse is a profoundly distressing form of mistreatment that can occur within nursing home facilities. It involves any non-consensual sexual activity or harassment that targets residents, causing emotional distress, loss of dignity, and severe trauma.
- Emotional abuse encompasses acts that inflict psychological harm on residents. This may include intimidation, threats, humiliation, or verbal abuse. Such actions can lead to emotional distress, severe anxiety, and a deterioration in mental well-being.
- Psychological abuse: Similar to emotional mistreatment, psychological abuse involves tactics that cause emotional harm, often through manipulation or controlling behavior. Residents may be coerced into actions against their best interests or suffer mental anguish due to the negligent actions of care home staff.
- Financial exploitation is the misuse or theft of a resident's finances or property by staff members or other residents. Victims may experience sudden financial losses and severe emotional distress due to these unlawful actions.
- Nursing home negligence occurs when the facility fails to provide the necessary care to residents, leading to adverse health outcomes. Neglect can result in conditions such as bed sores, sudden weight loss, unexplained changes in a loved one's health, or even wrongful death.
Residents of caregiving homes and assisted living facilities, including those in Arizona, have specific rights to protect their health, safety, and dignity. These rights are supported by federal and state legislation and serve as a cornerstone for advocating for caregiving home residents.
- Federal and State Protections: Under the Nursing Home Reform Act and Arizona state laws, residents' rights include quality care, respect, privacy, and freedom from abuse and neglect. These laws provide a framework for ensuring that nursing facilities meet minimum standards of care.
- Legal Recourse for Rights Violations: Legal recourse is available When these rights are violated. This may involve reporting to regulatory authorities, seeking remedies through civil litigation, or contacting an attorney specializing in nursing home abuse for legal representation and advice.
Understanding and navigating the legal options available in cases of nursing home neglect and abuse is crucial for victims and their families. This knowledge empowers them to take appropriate action to seek justice and hold the responsible parties accountable.
Determining Neglect and AbuseDetermining whether an act constitutes neglect or abuse is a critical first step in legal proceedings. This involves assessing the actions or inactions of nursing home or assisted living facility staff members and facilities against established care standards.
Steps to Take if Abuse is SuspectedIf abuse is suspected, immediate steps should be taken, including documenting the evidence, reporting to the appropriate authorities, and consulting with a qualified nursing home abuse lawyer in Tucson to understand the legal implications and options.
Reporting Nursing Facility AbuseReporting incidents of nursing abuse isn't just a moral duty; it frequently carries a legal obligation. Knowledge of the reporting process and recognizing the critical importance of reporting promptly to state or federal authorities can be pivotal in ending mistreatment and commencing legal actions. These authorities include:
- Arizona Long-Term Care Ombudsman Program
- Local Law Enforcement
- National Center on Elder Abuse (NCEA)
- Arizona Adult Protective Services (APS) at (877) 767-2385
- Arizona Department of Health Services at (602) 364-2536
Taking legal action not only seeks justice for the victim but also holds negligent parties accountable for their actions. Many families have found solace and compensation through legal avenues, ensuring that their loved one's injuries and suffering do not go unnoticed or unaddressed.
Reporting abuse and neglect to the appropriate authorities, such as the Arizona Attorney General's Office or the National Center on Elder Abuse, is also a crucial step in ensuring the safety of caregiving home residents.
Pursuing Compensation and JusticeAbused victims and their families pursuing compensation and justice is an essential part of the healing and recovery process. These compensations are designed to cover the costs associated with the abuse and acknowledge the suffering of the victim.
In caregiving home abuse cases, victims can seek damages for the following:
- Medical expenses
- Pain and suffering
- Emotional distress
- In some cases, punitive damages
Holding nursing facilities and their staff accountable for abuse or neglect is vital. Legal action can compel facilities to improve care standards and prevent future abuse.
Empowering victims and families in Tucson involves providing them with the knowledge and resources to address and respond to abusive behavior effectively. Legal support plays a crucial role in this empowerment.
Hire a Tucson Nursing Home Abuse LawyerFor those facing the challenges of abusive behavior, partnering with our Tucson nursing home abuse lawyers can provide the necessary legal expertise and support.
If you suspect a family member has suffered from abuse or neglect in an assisted living facility, our nursing home abuse attorneys are here to help. At Nursing Home Law Center, LLC, we offer:
- Free consultation to evaluate your case
- Expertise in cases involving sexual abuse and financial exploitation
- A team of qualified personal injury attorneys who understand the intricacies of living facilities
Our law firm is committed to advocating for the rights of nursing home residents and ensuring that they receive the justice and respect they deserve. Call our nursing home abuse lawyers at (800) 926-7565 to ensure those held liable are brought to justice.
 Pima County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Pima County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
