legal resources necessary to hold negligent facilities accountable.
Lexington Nursing Home Abuse Lawyer
 Nursing home abuse is a serious and growing problem in the United States. Thousands of nursing home residents are victims of yearly physical, emotional, and sexual abuse.
Nursing home abuse is a serious and growing problem in the United States. Thousands of nursing home residents are victims of yearly physical, emotional, and sexual abuse.
Often, the abusers are nursing home staff members entrusted to care for these vulnerable individuals. Do you suspect elder abuse in Kentucky nursing homes? Do you know a nursing home resident suffering from neglect in a nursing home? If so, it is vital to take action immediately.
The first step is to speak with the affiliate Kentucky personal injury attorneys at Nursing Home Law Center LLC. They will review legal documents in the case and determine the best course of action for the legal issues of the nursing home resident.
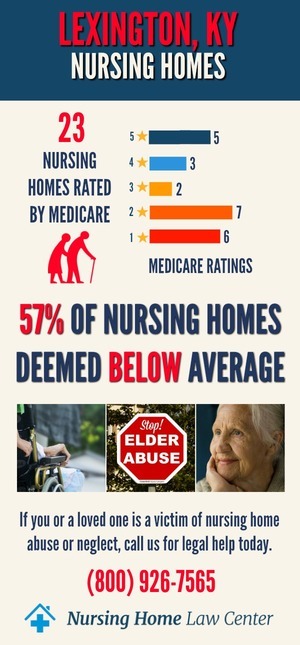
Don't wait until it's too late - contact Lexington nursing home abuse lawyers at (800) 926-7565 (toll-free phone number) to schedule a free consultation to determine your legal options.
An estimated 2.1 million people annually suffer from nursing home abuse or neglect, including physical, sexual, or emotional abuse, financial exploitation, malnutrition or dehydration. Often, the nursing home abuse victims are elderly and frail individuals who cannot protect themselves and rely on their caregivers for assistance and support.
Do you believe your loved one has been subjected to abuse or neglect in a retirement facility? If so, it is crucial to take action immediately. Accept our law firm's free consultation offer and speak to an experienced Lexington nursing home attorney to discuss your nursing home abuse case and how to take legal action.
Nursing Home ResidentsIt is crucial to ensure that the care of nursing home residents occurs in a comfortable and safe environment. They must be provided with the necessary assistance, proper care, and a supportive environment.
- Nursing home residents may require assistance with basic needs such as bathing, dressing, toileting, and other necessities. Sometimes, they may also require help managing their medication or completing exercises.
- A nursing home resident has rights under federal law, including being free from physical and mental abuse.
- A nursing home can be an excellent option for seniors who need ongoing care and assistance. Nursing homes provide residents with 24-hour skilled nursing care and access to therapy and other rehabilitation services.
- Seniors in nursing homes also benefit from being around people their age and can often make friends and socialize with others in the establishment.
- Nursing homes must meet specific standards of care to access federal funding. Unfortunately, not all nursing homes provide adequate care for their residents.
Retirement home abuse or neglect is a severe problem in the United States. Thousands of nursing home residents are injured, mistreated, or even killed in nursing homes each year. While most nursing homes provide quality care, too many facilities allow abuse and mistreatment of nursing homes.
When a loved one has been harmed through nursing home neglect, it is crucial to take action. You may file a lawsuit against the establishment or the abusers to recover damages. A nursing home abuse attorney can help you understand your legal options.
Causes of Kentucky Nursing Home AbuseAccording to the National Center on Elder Abuse (NCEA), one in 10 elderly Americans are victims of elder abuse each year. More than 5 million elders are abused, neglected, or exploited. There are many causes of retirement facility abuse and neglect. Some of the most common reasons are:
- Lack of staffing or understaffing
- Poor training or supervision of staff
- Poor working conditions
- Lack of respect for residents
- Lack of accountability
- Failure to report abuse
- Poor management
- Lack of resources
- Poor living conditions
- Substance abuse by staff
When there are not enough caregivers or staff members to attend to all the residents, the staff can become overworked and overwhelmed, leading to neglect and abuse
Where the retirement home staff is not adequately trained or supervised, they may be more likely to engage in abusive behaviors
When the work environment is stressful and chaotic, it can lead to frustration and anger resulting in abuse of the residents.
If the staff does not respect the residents, they may be more likely to engage in abusive behaviors
There might not be a system to hold the nursing home staff accountable for their actions; they may be more likely to abuse the residents
If the staff fails to report abuse, it can continue to happen.
When the nursing home facility is poorly managed, it can lead to several problems, including abuse.
When the long-term care facility does not have enough resources, such as money or staff, it can lead to mistreatment
If the living conditions are dirty and unsanitary, it can lead to residents being neglected
When the staff is abusing drugs or alcohol, they may be more likely to engage in abusive behaviors
Tell tale signs showing abuse of a nursing home resident may include:
- Sexual abuse or sexual assault involves anything from unwanted touching to rape
- Physical abuse consists of any form of touch where the resident suffered physical harm
- Psychological abuse or emotional abuse can include humiliation, intimidation, or neglect
- Financial abuse or financial exploitation is also common and may consist of stealing money or possessions from a nursing home resident.
Retirement home neglect is a serious problem that can cause significant injuries to a nursing home resident, including:
- Bruises: Elderly residents can easily bruise, especially if they are frail or have thin skin. Bruises can be a sign of physical mistreatment.
- Cuts: Scrapes could be a sign of physical abuse, primarily if they are located in places that would be difficult for the older person to reach themselves.
- Burns: Burns may indicate both physical and chemical mistreatment. They can be caused by scalding liquids, hot objects, or even cigarettes.
- Broken bones: Fractured bones could be a red flag of physical mistreatment
- Head or dental injuries
- Fatigue, insomnia, or other sleep disorders
- Dehydration and malnutrition
The following are the common types of nursing home abuse warning signs:
- Bruises, cuts, or other injuries that are unexplained or seem to have been caused by rough handling in nursing facilities
- Changes in mood or behavior, such as becoming withdrawn or aggressive
- Pressure sores or other signs of nursing home neglect
- Unexplained changes in financial situation, such as large withdrawals or unusual purchases
- Changes in appearance, such as weight loss or deterioration in personal hygiene
- Receiving unnecessary medication or being over-medicated
- Not receiving medical attention for wounds or illnesses
- Being isolated from friends and family
The federal government has nursing homes under scrutiny after recent reports of nursing home neglect. One such report led to the closure of a retirement home in Lexington, Kentucky.
The Lexington attorneys at Nursing Home Law Center have successfully represented many victims. If you suspect that your loved one is suffering at the hands of nursing home workers, it is time to stop nursing home abuse by reporting abuse and taking legal action.
We understand the unique circumstances surrounding a nursing home abuse case, and our law firm will work tirelessly to seek compensation for your suffering. Contact our law firm today for a free case evaluation.
Holding the Liable Party Accountable in Nursing Home Abuse CasesAn assisted living facility or retirement home in Lexington, KY, can be held liable if the negligence of a staff member results in an injury to a resident. The nursing facility could be held liable when the resident’s medical records show that the facility knew or should have known about the risks and failed to take steps to protect them.
In addition, the nursing facility may be held responsible if an employee or contractor committed the mistreatment. Our Lexington attorneys have represented numerous victims of nursing home neglect. We are committed to fighting for the rights of the elderly and holding abusers accountable.
How to File a Lexington KY Nursing Home Abuse LawsuitWhen you suspect abuse in a retirement home, taking swift and decisive action is vital.
- The first step is to contact a Lexington nursing home abuse attorney who can help you navigate the legal process and protect your loved one's rights and well-being.
- The second step is to file a complaint with the Kentucky Department of Public Health, triggering an investigation by the department, resulting in penalties for the retirement home.
- The third step is to file a civil lawsuit against the retirement home. The case can seek damages for your loved one's injuries and monetary compensation for their pain and suffering.
Average Settlement Amount in Kentucky Nursing Home Abuse Lawsuits
The average settlement is $323,000 in Kentucky nursing home abuse cases. The national median is $215,000, with settlements ranging from $50,000 to $1.5 million. The average jury verdict is $1.2 million in cases that go to trial.
Damages in Nursing Home Abuse Claims
In civil cases, damages are awarded to punish the wrongdoer and deter others from engaging in similar misconduct. Damages are not meant to compensate the victim for any losses suffered but to punish the defendant and send a message that this behavior will not be tolerated.
In nursing home abuse and neglect cases, damages may be awarded if the defendant's actions were particularly egregious or there was a history of similar mistreatment.
Legal Recourse For The Surviving Family Members After The Death Of A Family Member From Nursing Home AbuseHave you lost a loved one due to nursing home abuse and neglect? You may be wondering what legal assistance you can expect as a surviving family member.
Unfortunately, the answer to this question is not always straightforward. In some cases, it may be possible to file a wrongful death lawsuit against the retirement home, their insurance company, or the negligent party responsible for the mistreatment.
However, the laws governing wrongful death lawsuits vary from state to state, so it is essential to speak with a Lexington attorney in your area to learn more about your specific legal rights.
In some cases, the deceased victim's family may also file a personal injury lawsuit against the retirement home regardless of whether the victim died due to the mistreatment.
Typically, a personal injury lawsuit will result in financial compensation for the family's damages, including medical expenses, funeral and burial costs, and pain and suffering.
You may also seek punitive damages if the defendant's actions were particularly egregious or resulted in the death of your loved one.
Obtaining Legal Advice For Nursing Home Abuse Neglect And Physical AbuseRetirement home neglect is a serious issue. If you believe your loved one is being mistreated in a retirement home, it is crucial to get legal advice. A Lexington nursing home abuse lawyer can help you understand your rights and may help you file a lawsuit against the nursing home.
Elder abuse can take many common forms, including physical abuse, sexual abuse, emotional abuse, and financial abuse. It is important to remember that mistreatment does not always involve physical violence. If you are concerned that your loved one is being abused, it is vital to trust your instincts and get legal help.
The Lexington nursing home abuse lawyer can handle court costs, so no upfront payment is needed. You can focus on getting better and let us take care of the rest. We're here to help you seek the compensation you deserve.
Hiring a Lexington Kentucky Nursing Home Abuse Lawyer To Pursue A Nursing Home Abuse And Neglect CaseHave you been the victim of nursing home abuse and neglect? If so, our Lexington nursing home abuse attorneys have many years of combined experience representing clients and will help guide you through the legal process and fight to recover compensation for your suffering.
We understand how difficult this time can be, and we are here to support you every step of the way. Contact our law firm today toll-free at (800) 926-7565 or fill out a contact form for a free consultation and free case evaluation.
Contingency “No Win, No Fee” Guarantee
Each Lexington nursing home abuse attorney operates on a contingency fee basis, so you don't pay our law firm until we win your case.
All confidential or sensitive information you share with our legal team remains private through an attorney-client relationship throughout the free consultation and subsequent appointments.
Resources:
 Fayette County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
Fayette County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
