legal resources necessary to hold negligent facilities accountable.
Louisville Nursing Home Abuse Lawyer
 The Louisville nursing home abuse and neglect abuse attorneys are committed to combating the current rise in nursing home abuse cases. We use education and legal action to hold negligent nursing homes accountable for the misdeeds of their managers and employees.
The Louisville nursing home abuse and neglect abuse attorneys are committed to combating the current rise in nursing home abuse cases. We use education and legal action to hold negligent nursing homes accountable for the misdeeds of their managers and employees.
We encourage family members to research the Medicare violation history of any home they consider for their loved ones to ensure patient safety. Avoiding facilities with known nursing home abuse will not only protect those you care about, but it will also hurt the financial bottom line of these facilities that place profits over the well-being of their residents.
Was your loved one injured, abused, mistreated, or died unexpectedly from neglect while living in a nursing facility in Kentucky? If so, you have legal rights to ensure justice, and legal representation is only a call away. Do not allow the abuse to be left unchanged and unchallenged.
The affiliate Kentucky personal injury attorneys at Nursing Home Law Center LLC have the experience to help you recover damages from injuries or the death of a loved one caused by nursing home abuse or neglect.
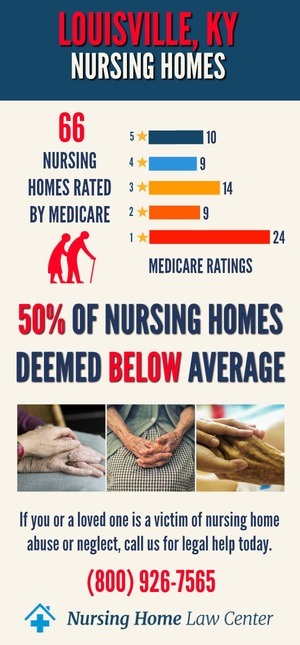
Each Kentucky nursing home abuse attorney at our law office can assist with providing comprehensive reviews of every nursing facility in the area, from five-star assisted living facilities to the lowest-rated long-term care facilities. Contact Louisville nursing home abuse lawyers at (800) 926-7565 (toll-free phone number) to schedule a free consultation and a no-obligation free case evaluation to discuss financial compensation in a personal injury suit.
Central Kentucky Senior DemographicsLouisville, Kentucky, is a city that was founded in 1778 by George Rogers Clark. Located to the west of Boston and Philadelphia, it's among one the oldest cities still standing today, with an aging population of 16% senior, which has increased demand for nursing homes throughout this region due primarily because they are vulnerable to abuse from other elderly citizens or staff members at these facilities if care isn't taken enough- especially when you consider how much money our nation spends on health care costs overall every year.
Central Kentucky Care Assisted Living Facility Violations & Safety ConcernsOur legal team thinks you have the right to information about the violations committed in nursing homes and facilities that will protect residents. These statistics will also assist you in avoiding placing your loved ones into unsafe environments where neglect and elder abuse are perpetrated in the nursing home.
By federal law, Medicare routinely collects data on every nursing facility in Kentucky based on information gathered through investigations, inspections, and surveys and makes the information public.
The publicly available database reveals that investigators found severe deficiencies and violations at fifty-eight (45%) of the 129 Central Kentucky nursing facilities, leading to nursing home abuse that caused injury or premature death to a nursing home resident.
When Can You Bring Legal Action Against Nursing Home Abuse?Many forms of Louisville nursing home abuse can be a reason to see an attorney regarding a personal injury case, but the most prevalent causes are listed below:
- Negligent Hiring
A nursing home can be held liable when they employ staff who cause elder abuse of residents, are unqualified to give quality care to a resident, or even if they are qualified, they still use their knowledge to manipulate the system to aid the perpetrator to cause harm to residents. Should a nursing home provide inadequate training, they are also liable. - Negligent Supervision
If the facility neglects to properly supervise its residents, it may be liable for negligent supervision of a nursing home. Should a resident at risk of falling not be adequately managed and fall and sustain injuries, the nursing home or facility may be at fault. - Neglect to provide a safe environment
Facilities must keep their premises safe. If it is found that they knew of possible danger and did not address it or if the staff played a part in causing dangerous circumstances, resulting in harm to a resident, the facility can be found liable. - Neglect to supply correct medical care
Nursing home facilities should provide the correct medical care to nursing home residents. Dispensing the wrong medication or failing to treat symptoms of illnesses and injuries could cause medical malpractice. - Neglect to provide clean and hygienic living conditions
Nursing homes fail when they neglect to keep their premises in a clean and hygienic condition at all times. Processes and procedures must be in place to ensure that standard common rooms and residents' private rooms are sanitary and safe.
Warning Signs and Injuries Seen In Nursing Home Abuse Cases
If you suspect that a family member or loved one is suffering from the abusive behavior of a Louisville nursing home staff member, watch for the below-mentioned signs associated with nursing home abuse.
Physical AbusePhysical abuse inflicts pain or injury upon a resident. It can include unnecessary confinement, restraints, or any other form of punishment such as rough handling or chemical restraints disguised as prescriptions. Unexplained injuries in a nursing home are considered a severe warning sign of elder abuse.
Other common signs of this physical abuse are:
- Bruises and lacerations
- Bed sores
- Restraint marks on wrists or ankles
- Broken bones
- Abrasions or laceration
- Burns
- Head and neck injuries
Emotional abuse of a nursing home resident often involves belittling, shouting, humiliating the resident, threats, manipulation and intimidation, and social isolation. Angry outbursts, depression, mood swings, and paranoia in the presence of caregivers are usual signs of abuse.
The following signs of emotionally abusive behavior:
- Regular disagreements between staff and nursing home resident
- Deep or unusual depression
- Changes in cleanliness and grooming habits
- Relationships that become strained or tense
- Sudden change in mental ability and alertness
- Fear of certain staff members at the nursing home facility.
- Unexplained withdrawal from usual or everyday activities
When nursing home residents are subjected to any form of sexual activity in a nursing home, including touching, rubbing, or intercourse, without their permission, they are suffering sexual abuse.
Vulnerable nursing home residents who have Alzheimer’s or dementia may be incapable of understanding that they are being sexually abused and are not capable of either consenting or refusing. Residents could also be threatened or forced to endure sexual abuse.
Typical signs to look for:
- Bruises on the skin of the breasts or genitals
- Sudden onset of a sexually transmitted disease (STD)
- Aggressive behavior and outbursts
- Signs of PTSD
- Emotional withdrawal and social isolation
- Suffering a pelvic injury
Nursing home residents are often the victims of financial exploitation regarding their money and personal possessions. It can include theft, misuse, and holding back of a resident's money or property. Data suggests that financial abuse accounts for over 2.6 billion dollars in costs for elderly Americans yearly.
Common forms of financial abuse include:
- Sudden changes in the resident’s situation
- Unusual or unexplained withdrawals from bank accounts
- Missing cheques, credit or debit cards
- Missing possessions and jewelry
When a staff member in a nursing home is negligent in their duty to give any resident necessities such as food, medical care, or health and bathing facilities, a resident has a case for nursing home neglect.
These are some of the signs of neglect:
- Bedsores - Treatment and prevention of bedsores are straightforward procedures. Your loved one may be a victim of neglect if nursing staff members cannot ensure that your loved one is repositioned regularly to prevent these sores or do not even notice the bedsores.
- Poor standards of hygiene -The development of an infection could be a sign of a lack of disease prevention measures, inadequate hygiene, or other negligent care. If the patient has a condition that worsens because the staff does not notice or report it, the infraction of nursing home neglect becomes even more severe.
Regardless of whether the neglect is willful or simply because overworked caregivers cannot tend to the needs of all their patients, the nursing facility needs to be held to account for acting in bad faith. Their inaction cannot be left unchanged.
Willful DispossessionAnother form of experiencing neglect is when a staff member intentionally refuses a nursing home resident food, medication, medical treatment, or therapeutic devices. This method of withholding or dispossession can cause the resident harm and be fatal.
Unexplained Infections or IllnessesThe development of an infection could be a sign of a lack of disease prevention measures, inadequate hygiene, or other negligent care. If the patient has a condition that worsens because the staff does not notice or report it, the infraction becomes even more severe.
Dehydration or MalnourishmentMalnutrition and dehydration could cause unexplained weight loss, darkened urine, lightheadedness, confusion, and weakness from a lack of proper care that could lead to wrongful death. Failing to prevent dehydration is a typical example of negligent care, and staff can be held liable for personal injury.
Unlawful RestraintSigns of forced restraint or bruises on the arms, legs, or genital areas could indicate physical or sexual abuse. Chemical and physical restraint measures are not legal without consent, but caregivers will sometimes break the rules to control unruly residents.
Victims of elder abuse suffer in silence, too afraid to speak up. They must endure the harsh circumstances of nursing home abuse, and the most important thing you can do to protect your loved one is to remain vigilant.
How to Help Victims?Don't just attribute the abovementioned signs of strange behavior or health conditions to old age; instead, investigate the nursing home conditions. Your loved ones might be victims of Louisville nursing home abuse; if so, contact Health and Family Services and report possible nursing home abuse cases.
You could also contact nursing home abuse lawyers and use our free consultation and free case evaluation to request legal assistance with an injury lawsuit.
Our free consultations offered by an attorney at our law office are available to any victim who has experienced neglect or abuse in a long-term care facility and wishes to hold the responsible party accountable for the harm caused to a family member or loved ones.
Nursing home abuse lawyers can open a personal injury lawsuit where those that neglected to properly care for loved ones can be held accountable. Family members of victims that suffered wrongful death can open a nursing home abuse lawsuit to claim compensation for medical expenses and other related costs.
Contact a Louisville Elder Abuse Attorney With Our Free Consultation Offer NowNursing Home Law Center, LLC represents nursing home neglect and abuse victims in nursing homes across the nation. We can help you determine the appropriate course of action for your loved one. Our only priority is your loved one's safety, and an attorney will help you decide whether or not they are the victim of abuse.
Each Louisville nursing home abuse lawyer at our law firm will take immediate action to remove your loved one from a nursing home abuse situation if necessary. From there, we can seek compensatory and punitive damages (if available) from the offending nursing homes for their unacceptable practices.
Let our affiliate attorney begin collecting the information we need to investigate your claim. Our Louisville law firm will review your legal options with you so that you know what to expect should you decide to proceed.
Contingency “No Win, No Fee” GuaranteeContact us today at (800) 926-7565 or use a contact form to arrange a free consultation with an award-winning Kentucky nursing home abuse and neglect attorney. Our free consultations offer is available to any person who has experienced neglect and wishes to hold the responsible party accountable for the harm caused to a family member or loved ones.
Each Louisville nursing home abuse attorney at our law firm works on a contingency basis to ensure you will pay us nothing until we've recovered compensation on your behalf.
Resources: Jefferson County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Jefferson County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
