legal resources necessary to hold negligent facilities accountable.
Independence Nursing Home Abuse Lawyer
 Moving a loved one into a nursing facility is never easy when families can no longer provide their loved ones with the necessary care. The families trust that they made the right decision in relocating their spouse, parent, or grandparent to a safe environment in a nursing home that provides loving and compassionate care.
Moving a loved one into a nursing facility is never easy when families can no longer provide their loved ones with the necessary care. The families trust that they made the right decision in relocating their spouse, parent, or grandparent to a safe environment in a nursing home that provides loving and compassionate care.
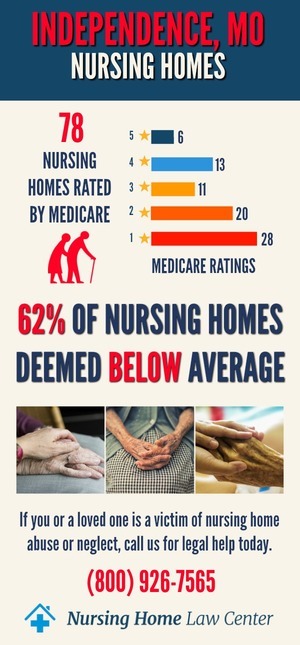
Was your loved one mistreated, or did they die unexpectedly from neglect while living in a nursing home in Missouri? Let our affiliate Missouri personal injury attorneys at Nursing Home Law Center, LLC protect your rights starting now. We have served many clients in the Independence, Missouri, area.
Contact our Independence nursing home abuse lawyers at (800) 926-7565 (toll-free phone number) today to schedule a free consultation to discuss how a lawyer from our law office can resolve a claim for compensation on your behalf to recover your damages.
What is Nursing Home Abuse?Nursing home abuse refers to mistreating a nursing home resident by a staff member or another resident. Unfortunately, abuse in nursing homes is not uncommon.
According to a National Center on Elder Abuse report, one out of ten American residents over 60 have experienced elder abuse. Unfortunately, most cases of elder abuse are not reported.
The NCEA reports that only one in 24 elder abuse cases are reported. That means that for every case of elder abuse that is reported, 23 cases go unreported.
There are many reasons why nursing home neglect or abuse victims might not report their mistreatment by others. Some victims may be afraid of retaliation from their abuser. Others may be unable to communicate what is happening to them in a nursing home due to physical or mental limitations.
Since the elderly depend on the nursing home staff for care and protection, they may be reluctant to report their caretakers to the authorities, fearing that they would not be believed.
Types of Nursing Home Abuse in Kansas City, MOAbuse in Kansas City, MO, nursing homes is a serious concern for families with loved ones receiving help from facility caregivers. The most common form of abuse and neglect involve:
Physical Abuse
Physical abuse is using physical force that injures or endangers the person. The type of abuse can involve:
- Slapping
- Pushing
- Kicking
- Punching
- Strangulation
- Use of a weapon
- Throwing objects toward someone
- Hitting a person with a hand or an object
- Hair pulling
- Choking
- Burning
Bodily abuse can have a long-lasting impact, even after the person has left the abusive situation. The effects of physical abuse may include:
- Chronic pain
- Headaches
- Stomach problems
- Sleep problems
- Anxiety
- Depression
- Post-traumatic stress disorder (PTSD)
In a nursing home, physical abuse can be committed by a caregiver, another resident, or a visitor. Signs include:
- Bruises, black eyes, scratches, and welts in various stages of healing
- Broken bones
- Sprains or dislocations
- Open wounds, cuts, or lacerations
Sexual Abuse
Any form of sexual contact or behavior that occurs without an individual's explicit consent is termed sexual abuse. It can happen to anyone, regardless of gender, age, or sexual orientation.
You should suspect nursing home abuse if you see the following signs:
- Bruises around the breasts or genital area
- Anal or vaginal bleeding
- STDs
- Torn, stained, or bloody underclothing
Has your family member been sexually abused in a nursing home? Take immediate action to ensure their safety is not compromised. Contact the police and the Missouri Adult Protective Services.
Emotional Abuse
Emotional or psychological abuse involves repeated words and actions that control, isolate, humiliate, scare, or degrade someone. Although psychological abuse doesn't cause physical injuries, it can have severe psychological effects.
Signs of psychological abuse include:
- Withdrawal from friends or social activities
- Loss of interest in hobbies or favorite activities
- Changes in eating or sleeping habits
A staff member or another resident could psychologically abuse your family member in a nursing home. Unfortunately, since there are no immediate visible signs of psychological abuse, it can be challenging to detect.
Any sudden changes in your loved one's behavior could indicate sexual abuse.
Financial Abuse
Financial exploitation can happen when someone uses their power to control another person's money without permission. Financial abuse can also occur when someone steals or misuses a nursing home resident's possessions or property.
Some signs of possible financial exploitation include:
- Sudden changes in a bank account or banking activity
- Missing money or valuables
- Forged signatures on financial documents, such as estate planning documents
- Sudden changes in a will or power of attorney
If you suspect your family member is being financially abused in a nursing home, you need to contact the police or file a report with Adult Protective Services. Such a nursing home abuse case requires the extensive intervention of lawyers, law enforcement authorities, and family members.
Nursing Home Neglect
Neglect is the failure of a caregiver to provide for the basic needs of a person under their care. It can include food, water, clothing, medical care, supervision, and emotional support.
Signs of neglect in a nursing home include:
- Pressure ulcers
- Dehydration
- Unattended medical needs
- Poor hygiene
- Dirty living conditions
The assisted living facility is responsible for providing care to your family member. If they fail to provide reasonable care, you can file a complaint with the facility's administrators or take the nursing home to court and receive compensation for the damages caused by their negligence.
Medical malpractice can also cause severe harm when a health care professional fails to follow protocols and provides sub-standard medical attention to a patient, leading to injury or death. Medical malpractice can take many forms, including misdiagnosis, surgical errors, failure to provide adequate medical attention, and more.
The Warning Signs of Nursing Home Mistreatment, Neglect, and AbuseMany families are unaware of apparent signs of abuse and neglect in nursing facilities.
Unfortunately, many residents suffer undue pain, abandonment, and intimidation. The National Center on Elder Abuse reports that there can be many signs of abuse in nursing homes. Some crucial signs to look for include:
Passive Neglect
Passive neglect usually involves a caregiver not providing adequate supervision, food, clothing, medical care, or other essential needs for the person under their care. In some cases, the neglect is so severe that it results in serious harm or wrongful death.
Confinement
Confinement refers to the staff's isolation or restraint of the elderly to protect the individual from harm. Although this practice is controversial, many facilities still use it to keep residents safe.However, federal regulations require a doctor to follow protocol and the law when ordering chemical or physical restraint. Any unauthorized use could be considered abuse.
There are many reasons why confinement may be used, including safety concerns, behavioral issues, and medical conditions.
However, if there are no medical reasons yet the nursing home staff is still confining or isolating the individual, it is considered psychological or emotional abuse.
Nursing home residents can become victims of physical or chemical restraint. Many are restrained without authorization as a convenience of the nursing staff or chemical restraints and over-medication to control resident behavior.
Pressure Sores
Every facility-acquired pressure sore (bedsores, pressure ulcers, decubitus ulcer) is preventable. However, bedsores can quickly degrade to a deadly condition without early detection.
Failing to follow protocol when managing skin care could be considered negligent behavior that leads to life-threatening injuries or death.
Willful Deprivation
It means the nursing home is not providing the resident with basic needs like food, water, heat, medical care, or access to the bathroom. For example, if a nursing home resident is not given enough food or water, it can lead to dehydration and malnutrition.
Have you noticed any signs of neglect or abuse? Consult nursing home abuse attorneys to hold the facility and caregivers financially accountable.
Legal representation is vital in a nursing home abuse case where the authorities are not taking any action against the perpetrators of abuse or are knowledgeable of the neglect at their facility.
The warning signs listed above are not in any order. Each type of neglect, mistreatment, and abuse can be equally harmful. Family members must take immediate action if suspicious that their loved one was mistreated.
What Makes Older Adults Vulnerable to Abuse?Many older adults are vulnerable to abuse because they are isolated from friends and family, have limited mobility, and may have cognitive impairments that make it difficult for them to access help or report abuse.
They may also depend on their abusers for care, making it even harder for them to leave an abusive situation. Some factors make older adults susceptible to abuse in nursing homes.
Cognitive Impairment
Older individuals with dementia or Alzheimer’s may be especially vulnerable to abuse. They may be unable to communicate what is happening to them or have trouble understanding what is happening around them.
Isolation
Older adults who do not have regular contact with friends or family members are at increased risk of abuse. They may be more likely to be victimized because their abusers know no one will check on them regularly.
Physical Impairment
Residents who have difficulty moving around or rely on others for help with activities of daily living are vulnerable to being abused since they cannot protect themselves. Their abusers may take advantage of their vulnerability and powerlessness.
Dependency
Some older adults depend on their caregivers for basic needs such as bathing, dressing, and eating. This dependency can make it harder for them to leave an abusive situation or get help.
How to Report Missouri (MO) Nursing Home AbuseWas your loved one a victim of abuse and neglect in a nursing home? Take the following steps to report the incident:
Step 1: File a Complaint with the Nursing Home Administrators
The nursing home administrators are responsible for the safety of your loved one and should be made aware of any abuse or neglect.
When you report an incident to them, ensure to include all relevant information about the neglect or abuse. Federal and state laws require the administrator to notify protective agencies that will start an investigation into what has occurred.
Step 2: Contact Adult Protective Services (APS)
Adult Protective Services (APS) is a state agency investigating elder abuse, neglect, and exploitation reports. In Missouri, you can contact the Adult Abuse and Neglect Hotline.
The Adult Abuse and Neglect Hotline responds to neglect, financial exploitation, and bullying reports. Call them at 1-800-392-0210. Once you file a statement, the Division of Regulation and Licensure will send an investigator to investigate the allegations.
Step 3: File a Police Report
Abuse and willful neglect are crimes. You should file a police report. The police will investigate the incident and may be able to press charges against the abuser.
To file a police report, you will need to provide the following information:
- The name and address of the nursing home
- The name and contact information of the victim
- A description of the personal injury
- The name and contact information of any witnesses to the abuse or neglect
After you file the report, get a copy for your records.
Step 4: Take Legal Action
Is the facility not following protocols to keep your loved one safe? You could file a compensation claim. You should consult with experienced nursing home abuse lawyers to discuss your legal options and the best way to protect the rights of your loved one.
Taking the legal route against a nursing home can be a complicated process. However, nursing home abuse attorneys can help you gather evidence, file the necessary paperwork, and represent you in court.
The first step is filing a complaint with the Missouri Department of Health and Senior Services. You can do this by mail or online.
Is the Nursing Home Taking Steps to Prevent Abuse and Neglect?Abuse in Missouri nursing homes is unfortunately not uncommon. When an older individual is admitted to a nursing home, the primary purpose is to ensure that they will be well taken care of by trained professionals.
There are numerous ways a facility administrator, Medical Director, Director of Nursing, and the caregiving staff can prevent abuse in Missouri nursing homes, including:
Hiring Trained Staff
Untrained staff can quickly become overwhelmed with their duties and may turn to abuse as a way to vent their frustration. All staff members should be adequately trained to handle the residents under their care.
They should know how to provide adequate care to the residents. Since many residents at nursing homes are suffering from one or more medical conditions, the staff should be familiar with the health care needs of the residents. Likewise, they should know what to do if there is an injury.
Regular Inspections
State officials should regularly inspect every nursing home to ensure they are up to code. The regulator should also ensure that the facility is providing reasonable care to the residents, especially when it comes to preventing abuse.
Hiring Sufficient Staff
Understaffed assisted living facilities are one of the main reasons behind abuse cases. Insufficient staff members who cannot provide adequate care to all the residents could overwhelm nurses and nurse aides, leading to an increased risk of resident injury, neglect, and abuse.
Are There any Criminal Penalties for Nursing Home Abuse?Most US states have laws that make elder abuse a crime. Depending on the state, penalties for nursing home abuse can range from a misdemeanor to a felony.
The penalties will also depend on the severity of the abuse. For example, if the abuse results in severe injury or death, the perpetrator can be charged with a more serious offense.
Penalties for nursing home abusive behavior can include:
- Jail or prison time
- Probation
- Fines
- Mandatory counseling or treatment
- Loss of professional license
You can check the Elder Abuse Guide for Law Enforcement (EAGLE) website to see what the laws are in your state. EAGLE is an online tool that helps officers, investigators, and prosecutors identify and investigate elder abuse cases.
Victims and family members have limited leverage to hold an abuser criminally accountable. Only law enforcement and the District Attorney can decide to charge someone for illegal actions.
Elder Abuse ResourcesOlder adults and their families can use the following resources to get more information about their legal rights or report abuse.
National Center on Law & Elder Rights
The National Center on Law & Elder Rights (NCLER) provides information, training, and technical assistance on legal issues affecting low-income older adults. NCLER also offers online and in-person training for paralegals and other professionals who work with older adults.
National Long-Term Care Ombudsman Resource Center
The National Long-Term Care Ombudsman Resource Center (NORC) provides state long-term care information and resources. Ombudspersons advocate for the elderly in nursing homes, assisted living facilities, and other long-term care settings.
Department of Justice Elder Justice Initiative
The Department of Justice Elder Justice Initiative is a resource for law enforcement, prosecutors, and service providers. The website includes information on elder abuse investigations, training materials, and research reports.
How Nursing Home Abuse Lawyers Can HelpHas your loved one experienced nursing home mistreatment, abuse, or neglect, and the facility did not take the required action? Speak with our lawyers to explore your legal options. Here's how a nursing home injury lawyer can help:
File a Personal Injury Case
Was your loved one injured due to nursing home mistreatment, abuse, or neglect? You could file a case against the at-fault party.
Our attorneys will help you determine if your loved one has a case and guide you through the filing process.
File a Wrongful Death Case
Any qualified family member can file a wrongful death lawsuit against anyone in the nursing home whose mistreatment, abuse, or neglect led to the death of a loved one. A preventable death case can help you recover compensation for your loved one, such as medical expenses, funeral and burial costs, and lost wages and benefits.
The main goal of filing a lawsuit is to get justice for your loved one. Our nursing home injury attorneys will provide the legal representation your family member needs to get the best possible outcome.
Receive Financial Compensation
Residents who experience abuse and neglect at nursing homes are also entitled to compensation. In addition, you can get economic and non-economic compensation for the negligence faced by your loved one. Monetary recovery might include:
- Economic Compensation - If the negligence of staff members or lack of proper care resulted in catastrophic injuries to your loved one, you might be able to receive economic damages. These monetary damages help with financial losses such as medical bills, lost wages, and future earnings.
- Non-Economic Compensation includes pain and suffering, mental anguish, and loss of consortium. You or your loved one may also be entitled to punitive damages designed to punish the at-fault party.
Our attorneys will work with you to determine the compensation your loved one may be entitled to and will fight to get you the maximum amount possible. Schedule a free consultation from a lawyer as soon as you suspect nursing home abuse.
Hire an Independence Nursing Home Abuse Attorney to Resolve a Compensation ClaimSpeaking out is vital when a nursing facility is providing substandard patient care. Legal action taken by our affiliate Independence abuse attorneys at Nursing Home Law Center, LLC, have brought to light many of the horrors of unsanitary conditions, poor quality of care, and abuse in Missouri nursing homes.
Was your loved one victimized by the nursing home staff, visitors, or other residents? Contact our law offices at (800) 926-7565 today. Schedule a free consultation to discuss the merits of your case and how best to proceed. No upfront fee is required.
All information our clients share with your lawyer is kept confidential as a part of our attorney-client relationship. We ensure our clients get the best legal representation to hold the nursing home accountable.
Resources:
 Jackson County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Jackson County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
