The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Can Bedsores Be Fatal?
Can bedsores be fatal? Unfortunately, yes—when nursing home residents are left immobile for long periods without proper attention, pressure ulcers, also known as bed sores, can form.
If nursing home staff members fail to reposition or assist residents who cannot move on their own, the skin can quickly break down, leading to painful and dangerous wounds. Without proper treatment, these injuries can worsen, becoming infected and potentially progressing to life-threatening complications such as bone infections, joint infections, sepsis, or even renal failure.
A nursing home bedsore lawyer can help family members secure justice for victims of negligent health care providers.

The Progression of Pressure Ulcers
Pressure sores vary in severity.
Stage 1
A stage 1 pressure sore occurs when lack of movement starts to affect blood flow. In the early stages, skin will develop non-blanchable redness, meaning it does not turn white when pressed. The skin is still intact and may feel warm; more severe cases may leave the skin purple or blue and this stage is more difficult to diagnose in people with darker skin.
Stage 2
Stage 2 decubitus ulcers will start to affect the integrity of the skin. The skin has partial thickness loss, which manifests as a partially open sore. These pressure injuries look like abrasions or blisters in the affected area. The skin itself will be discolored, and the area will be painful.
Stage 3
Stage 3 pressure ulcers involve a lot of dead tissue, which means skin thickness loss is occurring. The sore will look like a crater, and the edges of the sore may have dark patches of dead tissue. There may also be necrosis in the subcutaneous tissue, which means the deep wound penetrates the fat layer. Without proper medical care, they may become infected.
Stage 4
Stage 4 pressure injuries involve full-thickness tissue loss, exposing bones, such as shoulder blades, tendons, or muscles. The skin has been completely lost, creating serious risks of infection that can lead to death.

Bedsores Lead to Death and Other Risks
Decubitus ulcers are one of the most common signs of nursing home abuse or neglect. Here are a few risk factors associated with untreated sores that require prompt medical attention.
Infection
The most common complication of a skin sore is an infection. Bedsores lead to infections because a gap in the skin allows bacteria to pass through the skin barrier. Once the affected skin starts to break, the risk of a skin infectionincreases quickly. Nurses must prevent infection to avoid severe complications.
Sepsis
Sepsis is an extreme response by the body’s immune system. The more serious the infection, the harder the body must fight to defeat it. Essentially, the processes that are designed to fight the bacterial infection turn on the body instead, negatively affecting organs and other systems. This can lead to death.
Organ Failure
The final stage of a serious infection may be organ failure. In this scenario, the infection has led to sepsis and, eventually, septic shock. The body’s immune system is now attacking itself rather than the infection from the sore.
Prevention of Pressure Ulcers
Bedsores are caused by constant pressure on an area of the body, resulting in decreased blood flow that can deteriorate healthy skin and cause a sore. If you or a loved one is living in a nursing home, there are several ways to reduce the risk factors associated with decubitus ulcers.
Regular Skin Inspections
Frequent skin checks should become part of your routine, especially if you or your family member has reduced mobility or can’t sense pain.
Often, the affected skin may not feel painful during stage 1, so a visual inspection is the only way to notice the sore. Sustained pressure on the underlying tissue can lead to an open wound, which healthcare providers should look for. Fragile skin has a higher risk of breaking into an ulcer.
Pressure Relief Techniques
If a resident cannot move on their own and begins experiencing elevated pressure on a specific body area, it becomes the responsibility of nursing home staff to use pressure relief techniques that maintain healthy blood flow. Caregivers should regularly reposition residents to relieve pressure on vulnerable areas of the body.
For instance, if a resident has been lying on their back for too long, staff should gently adjust their position to the side. In addition, nursing homes and assisted living facilities can provide specialized mattresses and cushions designed to reduce pressure on bony areas while the resident is sitting or lying in bed, helping to prevent the development of painful and dangerous bedsores.
Adequate Nutrition and Hydration
The likelihood of developing bedsores increases if the skin is in poor health. Keeping skin healthy may delay the effects of a pressure ulcer. Patients should eat a balanced diet and stay hydrated.
Even if the patient develops a pressure injury, eating well and drinking plenty of water could prevent it from advancing. Speak with staff if you’re concerned about poor nutrition.
Skincare routines help prevent pressure ulcers and serious infections. Wash the skin’s outer layer well with soap and moisturize it. The cleaner your skin is, the easier it will be to prevent infections from sores. Even if it is too late to stop the ulcer, keeping the skin clean can aid in wound healing and keep the sore in its early stages.
Common Locations for Pressure Sores
Skin ulcers commonly develop in areas where bone and skin are in constant contact with a surface, leading to prolonged pressure and tissue damage. The most common affected areas are:
- Tailbone and buttocks – Due to prolonged sitting or lying down without repositioning.
- Shoulder blades and the back of the head – Common in bedridden residents (due to spinal cord injury or advanced age limitations) who aren’t repositioned regularly.
- Ankles and heels – Develop when legs remain in the same position for extended periods without support.
- Hips and lower back – Caused by improper repositioning or inadequate cushioning.

Legal Implications of Pressure Injuries
Nursing home patients suffering from an open wound due to poor blood supply and prolonged pressure are often victims of nursing home negligence.
The facility may be held liable if a nursing home resident dies or suffers the consequences of a severe infection from a pressure wound. Let’s discuss the potential legal implications of a skin sore in a nursing home.
Negligence and Malpractice
Medical professionals are required to provide a certain standard of care to patients. Elderly nursing home residents have the right to expect quality care, so if they develop severe pressure ulcers, it is often due to negligence or malpractice. These healthcare providers sometimes fail to ensure proper care for every resident, and an ulcer is an obvious sign that a resident is experiencing nursing home abuse and neglect.
Liability of Nursing Homes
Since nursing home staff are responsible for the health and well-being of residents, it is up to them to prevent developing pressure sores.
If nurses or administrators fail to prevent bedsores in a resident, the facility may be held liable for any legal damages. Legal damages in this type of case could include medical bills, emotional distress, physical pain and suffering, or loss of enjoyment of life.
Surviving family members can file a wrongful death lawsuit against the facility if pressure sores lead to death. Plaintiffs can claim damages for funeral costs, burial expenses, and loss of consortium.
Seeking Legal Advice
If you’ve noticed warning signs of poor circulation or advanced skin sores on a nursing home resident, legal action may be necessary.
Skin ulcers—especially in later stages—can lead to severe infections, sepsis, or even death. If you suspect negligence, consulting a nursing home abuse lawyer is critical. They can evaluate your case, help file complaints with facility administrators, and pursue legal claims for damages.
Victims and their families may be eligible to recover:
- Medical expenses – Covering treatment, hospitalization, and long-term care.
- Pain and suffering – Compensation for the resident’s physical and emotional distress.
- Punitive damages – If the facility’s negligence was particularly reckless.
- Wrongful death – If the neglect led to a fatal outcome, surviving family members may file a claim.
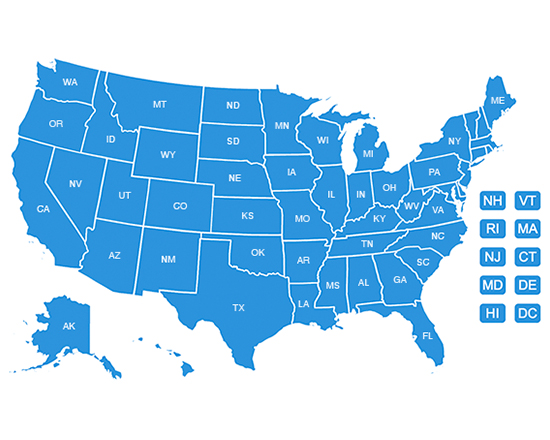
Statute of Limitations
The timeframe to file a nursing home abuse claim varies by state, typically ranging from one to three years from the date of injury or discovery. Missing this deadline could mean losing the right to seek compensation, so acting quickly is crucial.
Family members are often the first to notice signs of neglect. If left untreated, pressure sores can escalate quickly, leading to life-threatening complications. Seeking legal help immediately ensures your loved one’s rights are protected and increases the likelihood of holding the facility accountable.
What Is the Average Payout for Fatal Bedsore Cases?
According to Law.com’s VerdictSearch, payouts in fatal nursing home bedsore cases range from $55,169 to $114,000,000. The average payout is $5,800,570, while the median recovery is $1,208,740.
Several factors can influence the value of a claim, including:
- Stage and severity of the pressure ulcer
- Evidence of neglect
- Duration of suffering
- Causation
- Facility records
- Resident’s overall health
- Regulatory violations
Example Cases
$30,912,802 Verdict – Neglect Leads to Stage IV Bedsore and Death
Sam Rios Jr., 85, developed two heel pressure sores during a two-week stay at a skilled nursing facility. One progressed into a Stage IV wound that lasted nearly a year before his death. His family alleged severe neglect caused by chronic understaffing driven by corporate owners prioritizing profits.
The defense claimed the ulcers developed after discharge and were linked to underlying health issues. A jury found for the family, awarding over $30.9 million, including $25 million in punitive damages, wrongful death damages, and compensation for Rios’ suffering.
$29,100,000 Verdict – Failure to Prevent Bed Sore Causes Fatal Infection
Frances Tanner, 79, fractured her hip at a nursing home and was later hospitalized, where doctors also discovered a bedsore. Despite surgery for her fracture, she died when the sore became infected. Her daughter alleged reckless neglect and understaffing, asserting the sore originated at the facility due to a failure to reposition her.
The nursing home argued the sore developed after discharge. The jury disagreed, awarding $29.1 million, including $28 million in punitive damages, plus compensation for Tanner’s pain, suffering, and her daughter’s loss of companionship.
Consult an Experienced Attorney!
At the Nursing Home Law Center, we represent many clients who have suffered from pressure ulcers and sores. Our nursing home abuse lawyers will investigate your case, protect your rights, assess damages, gather compelling evidence, and even represent you in court if necessary.
The sooner you seek legal advice regarding the pressure injury, the sooner we can take action that could potentially save a life. We will also help you seek justice if you have already suffered due to the injury.
Call the Nursing Home Law Center today at 800-926-7565 or complete the online form to request a free consultation.