The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Towson Nursing Home Abuse Lawyer

Licensed in Maryland
Nursing home abuse is a deeply troubling issue that affects thousands of vulnerable residents in nursing homes and assisted living facilities across Maryland, including Towson. Families trust these facilities to provide a safe environment and proper care for their loved ones, yet abuse and neglect remain widespread concerns.
Seeking help from an experienced Towson nursing home abuse lawyer is essential to protecting the rights of the resident, pursuing justice, and holding responsible parties accountable. With the support of a skilled legal team, families can navigate the legal proceedings involved in abuse and neglect cases, helping them secure fair compensation for the harm caused.
Why Hire Nursing Home Law Center
At Nursing Home Law Center, we are dedicated to pursuing justice and fair compensation for victims of nursing home abuse. Our experienced legal team brings a strong record of handling nursing home abuse cases with care, achieving substantial settlements and verdicts.
We conduct thorough investigations to address every aspect of abuse, from medical expenses and emotional trauma to other damages suffered. With our extensive expertise in nursing home abuse claims, we manage the legal process efficiently and fight relentlessly to safeguard your rights.
Types of Cases Handled by Our Towson Nursing Home Abuse Lawyers
Nursing home abuse includes any form of neglect or intentional harm inflicted upon residents, leading to physical, emotional, or financial suffering. In Towson and throughout Maryland, nursing home abuse cases cover a range of situations, each impacting the health and dignity of vulnerable residents.
Our experienced nursing home lawyers handle various types of abuse cases, including:
Physical Abuse
Physical nursing home abuse involves intentional harm through acts like hitting, pushing, or using unnecessary restraints. This abuse can lead to visible injuries, such as bruises, cuts, broken bones, or other forms of physical trauma.
Mental and Emotional Abuse
Mental and emotional elderly abuse can cause severe distress and lasting psychological harm. This abuse may include verbal assaults, threats, intimidation, or isolation from social interactions. If a resident becomes withdrawn, anxious, or fearful around specific nursing home staff, it may be a sign of emotional or verbal abuse affecting their well-being and mental health.
Sexual Abuse
Elder sexual abuse involves any non-consensual sexual contact with a resident. Vulnerable and elderly residents are often defenseless against this violation, which can leave physical and emotional scars. Signs of sexual assault may include unexplained bruising, torn clothing, or sudden behavioral changes, particularly around certain caregivers.
Medical Malpractice
Medical malpractice cases occur when nursing home staff fail to provide adequate medical care, leading to preventable injuries or worsening health conditions. Common examples include untreated bedsores (pressure ulcers), medication errors, and failure to address serious medical needs.
Negligence
Nursing home negligence is the failure to provide essential care, resulting in harm to the resident. This neglect may include poor hygiene, malnutrition, dehydration, or elopement (when residents wander off unsupervised).
Financial Abuse
Financial abuse in nursing homes involves exploiting a resident’s finances for personal gain. This exploitation may include unauthorized withdrawals, coercing changes to financial documents, or theft of personal belongings.
Wrongful Death
When abuse, negligence, or medical malpractice results in a resident’s untimely death, families can pursue a wrongful death claim to seek justice for their loss. This claim allows families to hold the facility accountable for failing to ensure the safety and well-being of their loved ones.
Our Towson nursing home abuse lawyers are here to provide compassionate and effective legal representation for families affected by these types of abuse cases. We are committed to holding negligent facilities accountable and helping residents and families seek justice and compensation for the harm suffered.
Understanding Your Legal Rights
Nursing home patients are granted specific legal rights under both federal and Maryland state laws, which are designed to protect them from abuse, neglect, and exploitation. These laws require nursing homes and assisted living facilities to provide a safe, dignified environment for residents and hold facilities accountable when standards of care are violated.
The Nursing Home Reform Act of 1987 is a landmark federal law establishing quality standards for nursing homes receiving Medicare and Medicaid funding. This act grants nursing home residents the right to receive proper medical care, be free from physical and emotional abuse, and enjoy personal privacy and dignity.
Under this law, facilities that offer Medicaid services must adhere to certain standards, including proper nutrition, a clean environment, and access to medical and social services. Violations of these rights can lead to legal consequences for the facility.
In addition to federal protections, Maryland law enforces regulations to safeguard nursing home patients’ well-being. Maryland nursing homes must comply with strict staffing requirements, provide safe living conditions, and protect residents from financial exploitation.
State laws also support residents’ right to report concerns without fear of retaliation and ensure they receive proper medical and personal care.
Eligibility to File a Nursing Home Abuse Claim
When nursing home abuse, neglect, or wrongful death occurs, several parties are eligible to file a claim on behalf of the resident:
- The Resident: If capable, the nursing home resident can file a claim directly to seek compensation for harm and hold the facility accountable for any abuse or neglect.
- Family Members or Legal Guardians: Family members, such as children, spouses, or legal guardians, may file a claim on behalf of the resident, especially if the resident is incapacitated or unable to represent themselves.
- The Estate Representative: In wrongful death cases, the representative of the resident’s estate (often a family member or executor) can file a claim to seek justice and compensation for the loss suffered due to abuse or neglect.
Liability in Nursing Home Neglect and Abuse Cases
In nursing home neglect and abuse cases, liability may extend beyond individual caregivers to include nursing home management, the facility itself, and sometimes even external contractors or corporate owners. Holding all responsible parties accountable is crucial to ensuring that nursing home patients receive the proper care and respect they deserve.
Nursing Home Staff Members
Individual caregivers, nurses, and aides interacting directly with residents are often responsible for their day-to-day well-being. If staff members engage in physical abuse or neglect to provide proper care, they can be held liable for the resulting injuries and emotional harm.
Nursing Home Administrators and Management
Nursing home administrators and management teams oversee facility operations, hire qualified staff, and ensure that care standards are met. If inadequate training, poor hiring practices, or lack of supervision contribute to abuse, management may be liable for negligence.
The Nursing Home Facility
The facility can be liable for systemic issues like understaffing, lack of proper resources, or failure to adhere to federal and state regulations. For example, if a facility does not provide adequate staffing levels, which leads to neglect, the nursing home can be held responsible for failing to meet its duty of care.
Third-Party Contractors
Nursing homes sometimes rely on third-party contractors, such as medical providers or maintenance personnel, who may interact with residents. If these contractors fail to meet care standards and their actions injure residents, they and their employers may be held accountable.
Physicians and Medical Providers
Doctors, therapists, and other medical providers within the facility are responsible for delivering appropriate medical care. If a resident suffers due to medical malpractice, such as incorrect medication or untreated bedsores, these providers can be liable for failing to provide proper treatment.
Corporate Ownership
Many nursing homes are part of larger corporate entities that own and operate multiple facilities. The corporate owner may also be held accountable when corporate policies, such as cost-cutting measures, compromise resident safety and care.
Corporate decisions that impact resident well-being and contribute to abuse or neglect can lead to liability for the parent company.
How Our Towson Nursing Home Abuse Attorneys Can Help
With extensive experience in handling cases of nursing home abuse and neglect, our Maryland nursing home abuse attorneys are dedicated to protecting the rights of vulnerable residents and seeking justice for families impacted by abuse.
We understand the unique challenges of nursing home abuse cases and are committed to providing compassionate, effective representation. Our senior justice law firm has a strong record of success in securing compensation for victims.
Here’s how we can assist you and your family:
Free Case Evaluation
We offer a free, no-obligation case evaluation to help you understand your legal options. During this consultation, our attorneys will listen to your concerns, review the details of your case, and answer any questions you may have.
This initial assessment gives you clarity on the next steps and allows you to make an informed decision about pursuing a claim against the health care providers.
Case Investigation
Our legal team conducts a thorough investigation to gather crucial evidence that supports your case. This step includes obtaining medical records, facility documentation, witness statements, and other evidence to demonstrate the abuse or neglect suffered by your loved one.
By conducting a comprehensive investigation, we build a solid foundation to hold responsible parties accountable.
Filing the Claim
Once the investigation is complete, our attorneys take care of the formalities involved in filing a claim against the nursing home or assisted living facility. We handle all necessary documentation, ensuring that every aspect of the claim is carefully prepared and submitted within the legal timeframe.
By filing a well-documented claim, we strengthen your case and set the stage for a fair resolution.
Settlement Negotiation
In many nursing home cases, compensation can be achieved through settlement negotiations. Our attorneys are skilled negotiators who advocate for fair compensation to cover medical expenses, mental anguish, and other damages suffered by your loved one. We work diligently to secure a settlement that meets your family’s needs and reflects the full impact of the abuse.
Trial Representation
If a fair settlement cannot be reached, our legal team is fully prepared to represent you in court. With extensive trial experience, our attorneys will present a compelling case to seek justice for your loved one and hold negligent parties accountable. We are committed to pursuing every avenue to secure a fair outcome for your family.
Our Towson nursing home abuse lawyers are here to offer the guidance, representation, and support you need during this difficult time. Contact us today for a free consultation to discuss your case and learn how we can help your family seek compensation.
Common Signs of Elder Abuse Among Nursing Home Residents
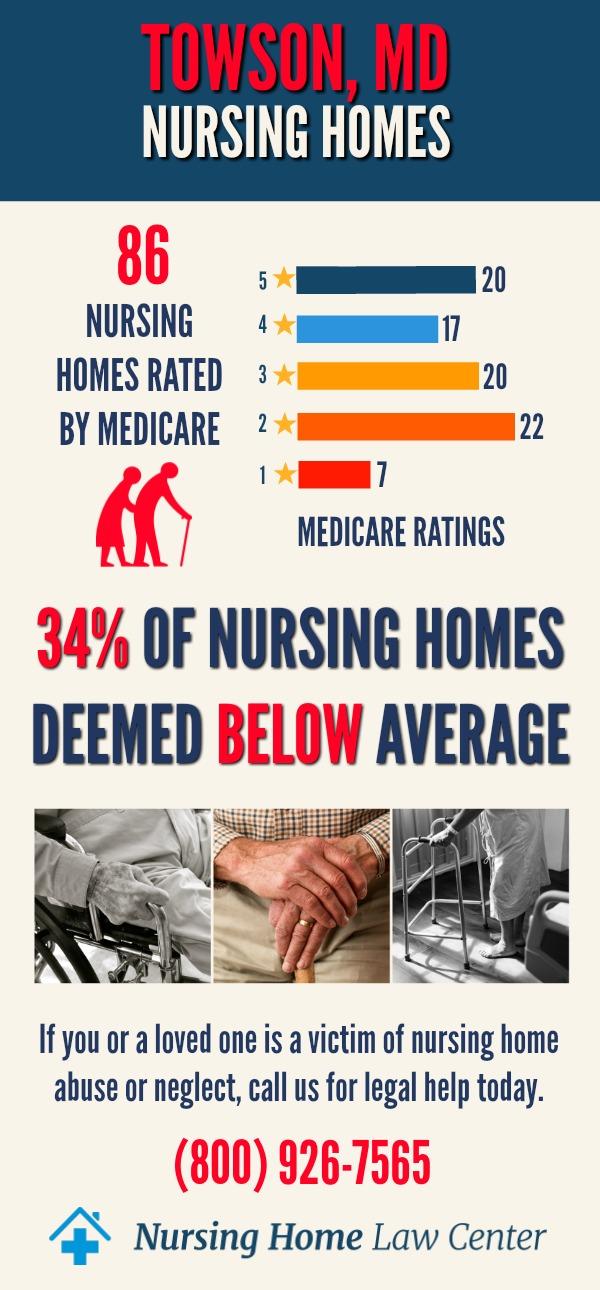
There are 93 Medicare-approved nursing homes in Towson, and many of them are struggling with their overall ratings and inspections. Specifically, 52% of these facilities have received an overall rating of below or much below average.
Health inspections are a critical concern, as 53% of nursing homes scored poorly in this category. This suggests widespread issues related to compliance with state and federal health regulations, potentially affecting residents’ well-being.
Staffing levels also present challenges, with 35% of facilities receiving below-average ratings. These staffing deficiencies reflect difficulties in providing consistent, adequate care for residents, impacting their day-to-day well-being and long-term health.
While 16% of nursing homes received low ratings in quality measures, this indicates that the majority of facilities maintain acceptable standards for resident care despite ongoing challenges with staffing and inspections [1].
The worst-rated nursing homes in Towson include:
| Autumn Lake Healthcare at Birch Manor | Autumn Lake Healthcare at Glen Burnie |
| Autumn Lake Healthcare at Homewood | Autumn Lake Healthcare at Loch Raven |
| Autumn Lake Healthcare at Pikesville | Autumn Lake Healthcare at Summit Park |
| Carroll Park Healthcare | Charlestown Community Inc |
| Complete Care at Heritage LLC | Courtland, LLC |
| Ellicott City Healthcare Center | Future Care Cherrywood |
| Future Care Cold Spring | Holly Hill Healthcare Center |
| Northwest Healthcare Center | Oakwood Snf LLC |
| Patapsco Healthcare | Peace Healthcare at Ridgeway Manor |
| Rossville Rehabilitation and Healthcare Center | Orchard Hill Rehabilitation and Healthcare Center |
Identifying signs of elder abuse in nursing home residents is crucial for families who want to ensure their loved ones are safe. Abuse can be physical, emotional, or even financial, and the signs aren’t always obvious. Understanding these indicators can help families take action to protect their loved ones.
Unexplained Physical Injuries
Physical signs of abuse can include bruises, cuts, broken bones, or burns that appear without explanation. For example, if a resident has frequent bruising or fractures, especially in areas not typically injured by falls, it may indicate physical assault or rough handling by the medical staff.
Sudden Behavioral or Emotional Changes
A shift in a resident’s personality or behavior—such as becoming withdrawn, anxious, or fearful—can indicate mental or emotional abuse. If a previously social resident suddenly becomes reclusive or appears frightened around specific caregivers, this change could be a response to verbal threats, intimidation, or isolation.
Poor Hygiene and Unsanitary Living Conditions
Nursing home negligence can result in poor hygiene, such as soiled clothing, unwashed hair, or dirty bedding. For instance, if a resident who previously maintained good hygiene now appears unkempt or lives in unsanitary conditions, it may suggest neglect, especially if there are visible issues like unclean bathrooms or lack of basic hygiene supplies.
Malnutrition and Dehydration
Malnutrition and dehydration can signal severe neglect. Signs of malnutrition or dehydration include rapid weight loss, dry skin, or extreme fatigue.
Bedsores and Pressure Ulcers
Bedsores, also known as pressure ulcers, develop when residents are left in the same position for prolonged periods without assistance. These sores are often painful and, if untreated, can lead to infections. Bedsores are a clear sign of neglect, as they are generally preventable with regular repositioning and attentive care.
Financial Irregularities
Financial abuse can involve unauthorized access to a resident’s finances, resulting in unusual bank withdrawals, missing personal items, or unexpected changes to financial documents. If family members notice discrepancies in accounts or find valuables missing, it could suggest financial exploitation, particularly if the resident appears unaware of the transactions.
Social Withdrawal and Isolation
If a resident suddenly becomes isolated or is discouraged from contacting loved ones, it may be an attempt by staff to control and conceal abusive behavior.
Signs of Sexual Abuse
Victims of sexual assault often show both physical and psychological symptoms. Signs may include unexplained bruising around sensitive areas, torn clothing, or behavioral changes, such as increased fearfulness or anxiety around certain staff members.
Untreated Medical Conditions
If a resident’s wounds or infections go untreated or chronic conditions are ignored, this may indicate neglect and a lack of proper medical attention within the facility.
If you notice any of these signs or serious injuries, it’s important to act quickly to protect your loved one. Consulting with a Towson nursing home abuse lawyer can help you explore your legal options and take steps to investigate and address any suspected abuse or neglect.
What to Do If You Suspect Nursing Home Abuse
If you believe your loved one may be experiencing abuse or neglect in a nursing home, taking immediate action is essential to protect their safety and well-being. Here are the steps to follow:
Call 911 if There’s Immediate Danger
If you suspect your loved one is in immediate danger or has suffered a serious injury, call 911. Emergency responders can provide necessary assistance, ensure your loved one’s safety, and create an official record of the incident.
Report to the Nursing Home Administrator or Management
Notify the nursing home administrator or management about your concerns. Management is legally obligated to address complaints of abuse or neglect and take corrective measures. Be sure to document your complaint and record any responses or actions taken by the facility.
File a Complaint with Your Local Ombudsman’s Office
In nursing home cases, the Ombudsman’s office advocates for the rights and well-being of home residents. Filing a complaint with your local Ombudsman can prompt an independent investigation into the facility’s practices and create a formal record of your concerns.
Ombudsmen work with nursing homes to resolve issues and ensure residents’ rights are protected.
Contact a Nursing Home Abuse Lawyer
Consulting with an experienced nursing home abuse lawyer is a critical step to protecting your loved one’s rights and seeking justice. A lawyer can guide you through the legal process, help gather evidence, and pursue compensation for any harm caused. Their legal support provides essential resources and peace of mind during this challenging time.
Taking these steps can help safeguard your loved one’s safety and initiate a process to hold the responsible parties accountable for any abuse or neglect they may have suffered.
Damages You Can Recover Through a Nursing Home Abuse Claim
If a loved one has suffered abuse or neglect in a nursing home, filing a claim can help your family seek justice and compensation for the harm endured. A successful nursing home abuse claim may cover different types of damages, each addressing specific aspects of the abuse and its impact on the victim and their family.
Economic Damages
Economic damages are financial losses directly related to the abuse or neglect. These may include:
- Medical Expenses: Costs for medical treatments, hospitalization, medications, and rehabilitation needed due to the injuries from abuse or neglect.
- Relocation Costs: Expenses involved in transferring the resident to a safer facility or arranging alternative care options.
- Ongoing Care: Fees for specialized in-home care or therapies required as a result of injuries or trauma inflicted at the nursing home.
Non-Economic Damages
Non-economic damages compensate for the emotional and physical suffering resulting from abuse or neglect. These may include:
- Pain and Suffering: Compensation for physical pain endured from injuries, such as broken bones or bedsores.
- Emotional Distress: Damages for the psychological impact, including anxiety, depression, or post-traumatic stress caused by abusive or neglectful treatment.
- Loss of Enjoyment of Life: Compensation for a decline in the resident’s quality of life due to abuse, which may prevent them from enjoying activities they previously found fulfilling.
Punitive Damages
Punitive damages may be awarded in cases where the abuse or neglect was particularly malicious, reckless, or intentional. These damages serve to punish the facility or responsible party and act as a deterrent to prevent future abuse.
Wrongful Death Damages
If abuse or neglect leads to the death of a nursing home resident, family members may file a wrongful death claim. These damages may include:
- Funeral and Burial Expenses: Compensation to cover the costs associated with funeral and burial services for the resident.
- Loss of Companionship: Damages for the emotional impact of family members due to the resident’s untimely passing.
- Loss of Financial Support: Compensation for any financial contributions the resident provided to their family, such as pensions, benefits, or savings.
Contact a Towson Nursing Home Abuse Attorney Today!
Our experienced team at Nursing Home Law Center is dedicated to protecting the rights of nursing home residents and securing justice for families affected by abuse and neglect.
With a strong track record in handling Maryland nursing home neglect cases, we have successfully helped clients achieve compensation for medical expenses, emotional trauma, and other damages suffered due to negligent care.
Our compassionate approach and commitment to holding facilities accountable make us a trusted choice for families seeking support and guidance.
If you suspect that a loved one has been subjected to abuse in a Towson nursing home, don’t wait to take action. Call us at (800) 926-7565 or fill out our contact form to get started.
References: [1] Medicare