The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Stage 3 Pressure Ulcer
Pressure ulcers are painful, uncomfortable, and dangerous to nursing home residents. They require constant care and monitoring — or they may worsen and threaten residents’ lives.
Healthcare providers use a four-stage system to determine the severity of a bed sore and establish a treatment plan. This article will describe pressure sores at stage three, the connection between neglect and pressure injuries, and what you can do if this situation affects you or a loved one.
What are Pressure Ulcers or Pressure Sores?
Pressure ulcers, also known as bed sores, are skin and underlying tissue injuries caused by prolonged pressure on one area. As the pressure restricts blood flow, skin cells become deprived of oxygen, suffer damage, and die off. This leads to open wounds that become worse with time if left untreated.
Pressure sores are common in nursing home residents who are immobilized and spend a lot of time in one position, whether that’s lying in bed or sitting in a wheelchair. They usually affect shoulder blades, hips, tailbone, heels, elbows, and other bony areas.
Stages of Pressure Ulcers
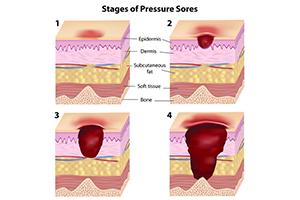
There are four stages of decubitus ulcers, determined by the level of tissue damage:
- Stage one – The skin is red, and it doesn’t become white when pressed for a few seconds. Although it may itch or hurt, the skin is still intact. They are harder to see on darker skin.
- Stage two – There’s partial-thickness skin loss with an open wound or blister, affecting the first two layers of the skin. The tissue underneath is intact.
- Stage three – Stage three pressure sores are deeper, and there may be necrotic (dead) tissue present.
- Stage four – The wound is deeper, exposing muscles, tendons, and bones. The tissue loss and infection risk are severe.
It is also possible to have a deep-tissue injury underneath intact skin, which is considered unstageable.
Stage 3 Pressure Ulcer: In-Depth
Stage three pressure injuries are serious and require quick medical attention. In some cases, the blood flow has been restricted for so long that the tissue has become necrotic.
Characteristics and Risk Factors
A stage three pressure sore presents with full-thickness skin loss, meaning the wound penetrates through the epidermis and dermis to reveal the subcutaneous tissue underneath.
While the fat tissue is exposed, bone, muscle, and tendons are not visible, although the risk exists. The wound bed may appear reddish or pink, with yellowish or grayish areas of slough (dead tissue). The entire pressure injury may look like a crater, with possible tunneling (where the wound extends deeper through the body like a channel).
The main pressure sore risk factors are:
- Old age
- Limited mobility
- Prolonged bed rest
- Poor nutrition
- Poor hygiene
- Incontinence
- Obesity
- Smoking
- Chronic health conditions such as diabetes and vascular issues
- Not moving, which restricts blood flow
Complications
Pressure injury complications can arise due to a lack of treatment, and can be life-threatening. They include:
- Joint infections
- Bone infections
- Sepsis
- Cellulitis (inflammation of tissue)
- Abscesses
Treatment
Treating pressure sores involves:
- Wound care – This includes debridement, or removal of dead tissue, to reduce the infection risk, as well as specialized dressings to prevent further injury.
- Relieving pressure – This can be done through frequent repositioning, specialized mattresses, cushions, and foam dressings to ensure proper blood supply throughout the body.
- Fighting infection – Pressure injuries can cause life-threatening infections. Caretakers must prevent them through proper care, and treat them with proper antibiotic therapy if they happen.
- Improving nutrition – A diet rich in protein, vitamins, and minerals supports wound healing and improves the body’s immune response.
- Skincare – Skin must be kept clean and moisturized, as dry, damaged, inflexible skin is more prone to pressure sores. This is especially true if the patient is incontinent.
- Surgery – Extensive stage 3 ulcers may require surgery to cover the wound or repair damaged tissue. It may be necessary to fight infection, especially osteomyelitis, to avoid life-threatening complications.
Negligence and Liability in Nursing Homes
New or worsened stage 3 pressure wounds can sometimes point to nursing home neglect. To prove that the home was negligent and recover compensation, you must show that it was directly responsible for the harm.
Duty of Care
The facility has a legal duty of care to ensure the safety and well-being of each nursing home resident, meaning it must also prevent bedsores.
Nursing homes must adhere to federal and state regulations on managing and preventing stage 3 pressure sores. This includes creating and implementing assessment and care plans for each resident, having sufficient and adequately trained staff, monitoring patients for pressure ulcers, and documenting the care.
If stage 3 pressure ulcers develop, the facility must do everything to prevent complications.
Breach of Duty
We can discuss nursing home negligence when long-term care facilities fail to comply with healthcare standards, and the violation causes preventable harm.
Nursing homes can breach their duty of care by failing to follow protocols such as regular skin assessments, repositioning residents, or maintaining adequate hygiene. When this breach results in harm, the facility can be liable for damages.
Causation and Damages
To hold the nursing home responsible, you must prove that its actions or inactions directly harmed the resident, such as resulting in a stage 3 pressure ulcer. For example:
- The staff failed to change the positions of the patient
- Their wounds were left untreated
- They weren’t monitored regularly
To establish a direct link, you can use evidence such as medical records, expert opinions, video footage, facility records, and witness testimonies. Aides can testify that the stage 3 ulcer slowly developed. A stage 3 ulcer is usually listed in medical records, too.
The final element of negligence is damages. You must demonstrate that the facility’s negligence led to damages, such as injuries, bacterial infections, distress, or medical bills. All of these are common in stage 3 ulcer cases.
Signs and Symptoms of Neglect
Nursing home residents may be unwilling or unable to speak up if they’re facing nursing home abuse or neglect. This is why families need to notice the signs and symptoms.
Physical Indicators
A stage three pressure sore can be a sign of neglect. Other physical signs to pay attention to are:
- Malnutrition – Significant, quick, or unexplained weight loss can point to neglect. The person may be weak and fatigued.
- Dehydration – A dehydrated person can exhibit dry skin, cracked lips, lethargy, and concentrated urine.
- Poor hygiene – Noticeable dirt, bad odor, or skin irritation can indicate poor hygiene and incontinence care.
Behavioral Changes
Vulnerable nursing home residents may be worried that if they ask for help, the situation may get even worse for them. However, some changes in behavior may indicate neglect:
- Withdrawal – Residents may become less social, avoiding interactions with staff or other residents.
- Depression – Signs may include persistent sadness, lack of interest in activities, changes in appetite, and difficulty sleeping.
- Agitation – Increased irritability, restlessness, or mood swings may signal frustration or discomfort from neglect or inadequate care.
The Role of a Nursing Home Injury Lawyer
If someone you love has suffered a stage three ulcer, it may be a red flag for neglect. Nursing home abuse lawyers can help you investigate the situation, file a claim against the facility, negotiate with the insurer, and, if needed, represent you in court.
Investigation and Evidence Gathering
Nursing home injury lawyers have experience with situations involving stage 3 pressure sores, so they will know how to investigate the pressure ulcer’s circumstances. They will support your claim through strong evidence, including:
- Medical and facility records
- Interviews with nursing home staff and other witnesses
- Photographic evidence
- Expert opinions
- Documentation of staffing levels and facility procedures
Negotiation and Settlement
Once they build a solid case, the nursing home attorney files a claim and negotiates with the facility and insurance company. Insurers sometimes minimize or negate the damages, but it’s harder for them if the plaintiff has skilled legal representation.
With extensive evidence and tried negotiation strategies, they increase your chances of reaching a fair settlement. Most nursing home injury lawsuits are settled outside court during the negotiation process.
Litigation and Trial Advocacy
If you’re not satisfied with the settlement, your nursing home neglect lawyer can take the nursing home to court, where they will represent your interests, examine witnesses, challenge the other party’s arguments, and present evidence.
An experienced lawyer will ensure you feel supported through the process, managing deadlines and other procedural matters so you can focus on resolving the trauma that the facility inflicted on your family.
Seeking Compensation for Damages
Family members and residents typically recover the following damages:
- Medical expenses – This includes the cost of treatments, surgeries, medication, and ongoing wound care throughout the healing process.
- Pain and suffering – You may recover damages for the pain and discomfort experienced due to the pressure injury. A patient safety issue often results in anxiety.
- Emotional distress – This includes damages or psychological impact, including anxiety, depression, and loss of quality of life.
- Punitive damages – In cases of gross negligence or intentional misconduct, you may be awarded punitive damages. Punitive damages exist to punish the facility and deter others from acting similarly.
Secure Expert Legal Counsel!
Nursing homes must ensure patient safety, dignity, and quality of care.
This includes following an evidence-based handbook, ensuring high-risk patients with health conditions don’t remain in the same position for long periods, and taking other actions necessary to prevent bedsores. If you suspect that staff members or management failed to fulfill this obligation, you have legal options.
If you’re unsure how to proceed or whether you have a case, contact a nursing home neglect lawyer. Call the Nursing Home Law Center at (800) 926-7565 or complete our online form to schedule a free consultation.