The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Henderson Nursing Home Abuse Lawyer
Nursing home abuse is a serious and growing concern, impacting vulnerable residents across Henderson and Nevada. Families place their loved ones in nursing homes expecting compassionate care, yet many elderly residents experience various forms of abuse, leading to a decline in overall health and well-being.
Seeking help from an experienced Henderson nursing home abuse lawyer is essential for the victim and their family. An attorney with expertise in nursing home abuse cases can help investigate the situation, identify responsible parties, and hold nursing home operators accountable.
Legal representation ensures that victims receive the justice and compensation they deserve while also helping to protect other residents from future harm.
Why Hire Nursing Home Law Center
At Nursing Home Law Center, we are dedicated to obtaining justice and fair compensation for victims of nursing home abuse. Our skilled legal team has a strong record of handling personal injury cases with care, achieving substantial settlements and verdicts for our clients.
We conduct comprehensive investigations to address every aspect of the abuse, including medical costs, emotional suffering, and other damages. Drawing from our extensive experience in nursing home abuse claims, we manage the legal process efficiently and advocate relentlessly to protect your rights.
Types of Cases Handled by Our Henderson Nursing Home Abuse Lawyers
Nursing home abuse involves any act or neglect that harms or exploits elderly residents in care facilities. This mistreatment can take many forms, impacting residents physically, emotionally, and financially. Our nursing home abuse lawyers handle a wide range of cases, helping families seek justice and compensation for their loved ones.
Physical Abuse
Physical abuse includes any intentional use of force that causes injury to a nursing home resident. This bodily assault can involve hitting, slapping, pushing, or the improper use of restraints. The misuse of restraints, either physical or chemical, can cause severe mental and physical pain.
Mental and Emotional Abuse
Mental and emotional abuse refers to actions that cause psychological harm to residents. This abuse may not leave visible signs but can lead to severe mental distress. Examples include verbal insults, humiliation, threats, and isolating residents from others.
Sexual Abuse
Sexual abuse involves any non-consensual sexual contact or behavior directed at a resident. This type of abuse is especially traumatic, as many residents may be physically or mentally unable to defend themselves or report the abuse. Such abuse can include inappropriate touching, forced nudity, or sexual assault.
Medical Malpractice
Medical malpractice occurs when nursing home staff fail to provide adequate medical care, leading to harm. Examples include untreated bedsores (pressure ulcers), medication errors, and failure to address health concerns.
Negligence
Nursing home neglect refers to a failure to provide essential care, often resulting in harm to the resident. This neglect can include poor hygiene, inadequate nutrition, dehydration, and lack of supervision. Negligence can also lead to elopement, where residents with cognitive impairments wander away unsupervised, posing significant risks.
Financial Abuse
Financial abuse involves exploiting a resident’s finances for personal gain. This abuse can include theft, unauthorized access to bank accounts, or pressuring residents to sign over assets.
Wrongful Death
Wrongful death may result from untreated infections, severe falls, medication errors, or other failures in care. Families may pursue wrongful death claims to hold the facility accountable and seek justice for their loved ones.
Understanding Your Legal Rights
Federal and state laws safeguard nursing home residents’ rights to dignity, safety, and proper care.
The Nursing Home Reform Act of 1987 is a landmark federal law designed to protect the rights of nursing home residents. Enacted as part of the Omnibus Budget Reconciliation Act, this law sets out minimum care standards for all nursing homes receiving federal funds through Medicare and Medicaid.
In addition to federal laws, Nevada state laws provide further protection to nursing home residents. Nevada requires that nursing homes adhere to strict licensing standards, including staffing, safety, and health care protocols.
The Nevada Division of Public and Behavioral Health oversees nursing homes within the state, enforcing state-specific regulations that support resident rights and address violations.
Nevada law mandates that nursing homes provide a clean, safe environment with appropriate medical attention, adequate staffing, and access to resources to ensure each resident’s well-being. Residents and their families may file complaints with the state health department, which investigates allegations of abuse and enforces corrective measures when necessary.
Eligibility to File a Nursing Home Abuse Claim
If a nursing home resident’s rights have been violated due to abuse, neglect, or inadequate care, certain individuals may be eligible to file a claim to seek justice and compensation.
- The Resident: If physically and mentally capable, the resident can file a claim directly against the responsible parties for any harm they have endured.
- Family Members: If the resident is incapacitated or otherwise unable to act on their behalf, family members may step in to file a claim. These could include spouses, children, or legal guardians who are advocating for the resident’s well-being.
- Legal Representatives: If the resident has appointed a legal representative, such as a guardian or someone with power of attorney, that representative may file the claim on the resident’s behalf.
- The Estate of a Deceased Resident: In cases where nursing home neglect has tragically led to the death of a resident, the estate’s executor or a close family member may pursue a wrongful death claim to hold the responsible parties accountable.
Liability in Nursing Home Neglect and Abuse Cases
In cases of nursing home neglect and abuse, multiple parties may be held liable, depending on the circumstances surrounding the mistreatment.
- Nursing Home Staff: Individual caregivers and staff members are often the direct perpetrators in cases of abuse and neglect. Examples include staff who commit physical abuse, neglect to provide necessary care, or mishandling medication.
- Nursing Home Operators: The operators of a care facility are responsible for hiring, training, and supervising their staff. If abuse or neglect occurs due to inadequate training, lack of background checks, or failure to address complaints, the facility operator may be held accountable.
- Medical Staff and Contractors: Physicians, nurses, and other healthcare providers working in the facility are expected to deliver proper medical care. Errors such as misdiagnosis, improper medication administration, or failure to respond to health concerns can result in liability for medical malpractice.
- Maintenance and Housekeeping Services: Third-party contractors who provide maintenance or housekeeping services may also be liable if their actions or negligence contribute to unsafe conditions.
- Pharmaceutical Providers: In some cases, pharmaceutical providers who supply medication may be held responsible if improper medications are delivered, mislabeled, or stored incorrectly, harming the resident.
- Facility Management and Supervisors: Supervisors and management personnel who oversee daily operations must ensure resident safety and address potential risks. If they fail to monitor staff effectively or ignore signs of abuse, they may be liable.
How Our Henderson Nursing Home Abuse Attorneys Can Help
At Nursing Home Law Center, our team brings extensive experience in representing victims of nursing home abuse and neglect in Henderson. We are committed to advocating for the victim and their family, handling each case with the attention and care it deserves.
Our Nevada nursing home abuse attorneys have a proven record of securing compensation for clients and holding negligent parties accountable for their actions.
Free Consultation
We begin with a free consultation where we review the details of your case. During this evaluation, we listen to your concerns, answer your questions, and provide an honest assessment of your legal options. This first step helps families understand their rights and how our team can help without any upfront costs.
Case Investigation
Our personal injury lawyers conduct a comprehensive investigation into the circumstances surrounding the abuse or neglect. This process includes gathering medical records, interviewing witnesses, reviewing staff backgrounds, and examining facility inspection reports.
Our team works to uncover every detail and piece of evidence needed to build a strong case, holding all responsible parties accountable for their actions.
Filing the Claim
Once we have built a solid foundation, we handle all aspects of filing the claim. We prepare and submit the necessary legal documents in a timely manner, ensuring that your claim is fully documented and meets all legal requirements.
Filing the claim is an essential step in seeking compensation for damages such as medical expenses, pain and suffering, and emotional trauma.
Settlement Negotiation
In many cases, we can reach a fair resolution through settlement negotiations, sparing families from the stress of going to court. Our nursing home abuse attorneys are skilled negotiators who work to secure a settlement that reflects the full extent of your loved one’s injuries and the financial impact of the abuse.
Trial Representation
If settlement negotiations fail, our personal injury lawyers are prepared to take your case to trial. We present compelling evidence to seek justice for your loved one, drawing on our extensive courtroom experience. Our legal team remains dedicated to protecting your family’s interests and securing the best outcome, whether through settlement or trial.
Common Signs of Elder Abuse Among Nursing Home Residents
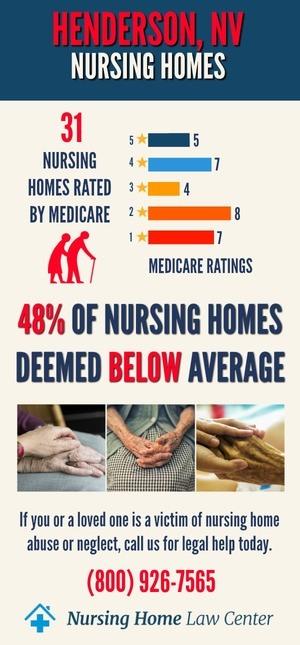
In Henderson, there are 42 Medicare-certified nursing facilities, with 11 facilities (26%) rated below or much below average overall. Specifically, 12 homes (29%) fall short in health inspections, and 18 homes (43%) have inadequate staffing levels. Nine facilities (21%) are rated poorly in quality measures. [1]
Abuse may not always be obvious, and residents may be unable or unwilling to speak up due to fear or cognitive impairments. Here are some common signs of elder abuse in nursing homes to look out for:
- Unexplained injuries, such as bruises, lacerations, broken bones, or burns
- Bedsores (pressure ulcers)
- Poor personal hygiene and unsanitary conditions
- Malnutrition and dehydration
- Fear of specific nursing staff
- Behavioral changes
- Financial irregularities
The worst-rated nursing homes in Henderson include:
| El Jen Skilled Care | Mission Pines Nursing and Rehab Center |
| North Las Vegas Care Center |
Contact a Henderson Nursing Home Abuse Attorney Today!
At Nursing Home Law Center, our experienced personal injury lawyers have a strong track record of fighting for justice on behalf of nursing home abuse victims in Henderson.
We understand the complex issues surrounding nursing home abuse cases and are dedicated to helping families hold responsible parties accountable. Our team has secured substantial settlements and verdicts, ensuring the victim receives fair compensation for their suffering and medical needs.
We work on a contingency fee basis, meaning you pay nothing upfront, and we only collect fees if we successfully secure compensation for you. If you suspect that your loved one has experienced nursing home neglect, don’t delay.
Call us at (800) 926-7565 or fill out our contact form for a free consultation to discuss your case and take the first step toward protecting your loved one.
References: [1] Medicare

