The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Nursing Home Diabetes Lawyer
Diabetes is becoming more common in the elderly, especially those in nursing homes. It’s estimated that 1 in 3 adults over the age of 65 have diabetes. [1]
Diabetes can cause significant health issues if not properly treated, including cognitive impairment, peripheral vascular disease, microvascular complications, coronary heart disease, urinary incontinence, weight loss, diabetic neuropathy, and more.
Read on to learn more about the unique risk factors of diabetes in the elderly, common health-related complications, and how you can hold nursing homes accountable if you or your loved ones experience complications.
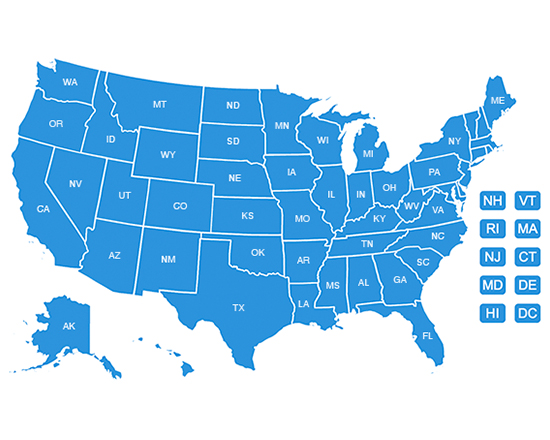
The Nursing Home Law Center can help you seek compensation for nursing home negligence.
Unique Risk Factors of Diabetes in the Elderly
Diabetes management can be challenging for many older adults, especially if they develop diabetes mellitus later in life. Elderly patients may face:
- Cognitive decline: Attention, memory, and thinking speed may naturally decline. This cognitive impairment can be a natural result of common geriatric syndromes, including dementia. Cognitive impairment can make it challenging for patients with diabetes mellitus to communicate with caregivers, hit glycemic targets, and maintain tight glycemic control.
- Multiple medications: Elderly adults may take several medications, which can interact with one another adversely. It may also be challenging for older adults with geriatric syndromes like Alzheimer’s to manage complicated medication regimens.
- Decrease mobility: Older adults may find it difficult to move. Decreased physical activity and mobility can adversely affect the body’s ability to manage glucose levels and make older adults more likely to develop microvascular complications.
Comorbidities can make diabetes difficult to manage in older adults. Nursing homes can create a diabetes prevention program, including a diabetes educator, to help older patients learn more about their disease. However, complications often arise when facilities don’t take extra steps to prevent them.
Common Diabetes-Related Complications in the Elderly
Diabetes may not have a significant impact on a person’s life if it is adequately managed with medication, diet, and lifestyle changes. However, if it is left untreated or mismanaged, diabetes increases the risk of serious complications.
Hypoglycemia (Low Blood Sugar)
Hypoglycemia is also known as low blood sugar. It can be caused by:
- Inadequate diet: Older patients may not eat enough carbohydrates, fat, protein, and fiber.
- Insulin: You can take too much insulin or take it at the wrong time
- Lifestyle: You may not have enough physical activity, consume alcohol, etc.
Symptoms of hypoglycemia include:
- Dizziness
- Headache
- Fast heartbeat
- Shaking
- Sweating
- Behavioral changes (anxiety, irritability, confusion)
Severe hypoglycemia in elderly diabetics can cause cognitive decline, physical disabilities, and increased mortality if not treated.
Older adults in nursing homes may have an increased risk of developing diabetes-related complications compared to younger patients, including hypoglycemia. If the staff does not routinely monitor their blood sugar levels, it can cause adverse outcomes.
Hyperglycemia (High Blood Sugar)
Hyperglycemia is caused by too much glucose in a person’s bloodstream. It’s also known as high blood sugar, and it can be caused by:
- Diet: Older adults can eat too many carbohydrates, which can cause their blood sugar to spike.
- Lifestyle: Lack of physical activity, stress, sickness, and injuries can also impact blood sugar levels. Older adults with mobility issues are more likely to have complications from diabetes compared to those who are more active.
- Medication: Elderly patients with diabetes may not take enough insulin or other diabetes management medications. Other medicines, like steroids and immunosuppressants, can also impact a person’s blood sugar levels.
Like hypoglycemia, hyperglycemia can impact a person’s long-term cognitive function and increase the risk of developing infections.
Foot Complications (Diabetic Foot Ulcers)
Diabetic foot ulcers are open wounds that develop on a diabetic person’s feet. They are similar to bedsores or pressure wounds, and they can occur because of:
- Nerve damage: People with diabetes may experience nerve damage and a loss of sensation in their feet. Because they cannot feel the pain, patients do not know they need to move their feet.
- Poor circulation: The lack of blood flow to the area can cause diabetic foot ulcers to appear and prevent them from healing in older patients.
- Lack of mobility: Patients with diabetes who are not active and sit in one spot for long periods can develop diabetic foot ulcers
These wounds can vary in severity and carry a high risk of developing infections, including sepsis. Sepsis is a type of blood infection that can cause organ damage and failure and may even lead to death. Additionally, the pressure wounds can develop gangrene and require amputation to stop the spread of infection.
Treatment of diabetic foot ulcers includes:
- Debridement: Doctors can remove the dead tissue. This will get rid of the infection and speed up healing. Dead tissues can be cut out, treated with enzymes, or washed with water pressure.
- Medication: Antibiotics and topical solutions may be used to treat infections in addition to daily wound care.
- Offloading: The pressure should be removed and redistributed to help restore blood flow and promote healing.
Diabetic foot ulcers and other foot complications may take time to heal and may cause a short-term functional disability. Glycemic control reduces the risk of foot ulcers.
Chronic Kidney Disease (Diabetic Nephropathy)
Diabetes or poor glycemic control can damage the kidneys over time, leading to diabetic nephropathy. This is a form of kidney disease, and it develops as a result of both type 1 and type 2 diabetes.
Kidney function deteriorates over time, leading to:
- Kidney damage: Diabetes can damage the kidney’s blood vessels. This may impact how your body filters waste from the blood and cause high blood pressure.
- Kidney failure: During end-stage renal disease (ESRD), your body may no longer be able to filter waste from the blood, causing waste and fluid to build up.
If you experience end-stage diabetic nephropathy, you may need dialysis for the rest of your life or a kidney transplant. While kidney disease can be managed with treatment to some extent, it can still impact your overall quality of life.
Eye Complications (Diabetic Retinopathy)
Diabetics can develop various eye complications, including diabetic retinopathy. This is when high blood sugar levels can damage the retina’s blood vessels. It’s a common comorbid illness, but if left untreated, these common complications can eventually lead to blindness.
Symptoms of diabetic retinopathy include:
- Changes in vision, including an inability to read or see far away
- Blurred vision
- Floaters or dark spots in your vision
- Seeing colors as faded or washed out
People with diabetes can help reduce the risk of developing diabetic retinopathy by controlling their blood sugar levels. Advanced bases may require laser eye treatment or surgery to help restore vision.
Cardiovascular Disease
Cardiovascular disease is the most common cause of death for the diabetic population. Older adults with diabetes may carry a higher risk of developing coronary disease, including:
- Coronary artery disease: Diabetes can impact blood flow to the heart.
- Congestive heart failure: The heart does not pump blood normally due to blocked arteries or heart damage.
- Stroke: Strokes occur when blood flow to the brain is reduced or blocked.
The longer a person has diabetes or doesn’t control blood glucose levels, the higher their cardiovascular risk. Heart disease can be fatal in older adults.
Nursing Home Negligence and Diabetes Complications
Nursing homes owe their patients a duty of care, especially those with diabetes and other comorbid illnesses. If they do not adequately manage their residents’ health, they can be held liable for complications.
Failure to Properly Monitor Blood Sugar Levels
Monitoring blood glucose is one way to prevent dangerous spikes and dips. Nursing homes should routinely monitor their residents’ blood glucose levels. If they do not, it can cause dangerous fluctuations and lead to serious long-term complications, including kidney damage, weight loss, eye deterioration, cerebrovascular disease, and more.
Medication Errors
Diabetes can be managed through medication and lifestyle changes. Increased activity can control cardiovascular risk and reduce associated risk factors in older patients. Insulin therapy is commonly used to control blood glucose levels.
However, nursing homes can give patients with diabetes incorrect dosages, incomplete treatment courses, and missed medications. These mistakes can disrupt an elderly patient’s diabetes management and lead to complications.
Inadequate Foot Care
Proper foot care is critical for diabetic residents as it is very easy for them to develop diabetic foot ulcers. Neglect, including improper hygiene, infrequent repositioning, and too-tight dressings, can lead to serious foot complications. Deep pressure wounds can develop and, if left untreated, may cause nerve damage or require amputation or other surgical intervention.
Failure to Address and Manage Complications
A nursing home is responsible for providing care to older adults with diabetes and managing coexisting chronic illnesses. Failure to promptly address and manage complications can lead to worsened health outcomes.
It can lead to more severe treatment options, increase suffering for residents, and cause death. However, facilities often put people with few coexisting chronic illnesses lower on the priority list, leading to complications.
The Role of a Nursing Home Injury Lawyer
If you or your loved one experiences diabetes complications while receiving care at a nursing home, you may be the victim of nursing home neglect. A nursing home injury lawyer can help you navigate your legal options.
Investigating Potential Negligence
A lawyer can help investigate the circumstances surrounding a resident’s complications, including:
- Medical records: They can look at your medical history, treatment plans, prescription medicine surgeries, and more to determine your health status before and after the complications.
- Witness statements: Lawyers can interview doctors, staff, residents, etc., to help get a picture of the living conditions and whether the facility used proper disease control procedures.
- Review documentation: Lawyers review complaints, investigation reports, and other documentation to help build your case.
This information can help them determine if negligence resulted in an increased risk of diabetic complications.
Holding the Nursing Home Accountable
Nursing home injury lawyers can help you hold nursing homes accountable for negligence, including helping you file a lawsuit to seek compensation for the damages you experienced.
To do so, you must establish the following four elements of negligence.
- Duty of care: The nursing home has a duty of care to you as a patient, especially as you manage your diabetes.
- Breach of duty: The nursing home did not live up to its duty of care, and you experienced complications as a result of their mismanagement of your diabetes.
- Causation: Their breach caused complications with your diabetes diagnosis.
- Damages: Due to these complications, you experienced significant damage to their well-being.
The damages patients with diabetes can recover depend on the circumstances of their case. They may include:
- Medical bills: Doctors visits, hospitalizations, medications, surgeries, and other medical costs associated with diabetes care can be recovered.
- Pain and suffering: Many older adults face significant physical pain and emotional suffering as a result of their diabetes.
- Punitive damages: If the nursing home is found guilty of gross negligence, you may be able to recover punitive damages. These damages are intended to punish the nursing home and deter them from acting in this manner again.
Nursing home injury lawyers can help you receive fair compensation as you navigate the aftermath of your diabetes complications.
Protecting Residents’ Rights
Your lawyer is your advocate throughout the entire legal process. They help protect residents’ rights and ensure their clients receive proper care and attention for their diabetes. If they do not, lawyers can help:
- Explain your legal options: Older adults may be overwhelmed by their legal options regarding mismanagement of their diabetes care. Lawyers can help you understand the best course of action to help you get justice.
- Represent you: Your lawyer can be your intermediary between the nursing home, lawyers, investigators, and more. They will speak for you so you can focus on healing.
- Negotiate fair settlements: They will advocate for a fair settlement based on your injuries. They will represent you during all legal proceedings if a settlement cannot be reached.
Nursing home injury lawyers strive to hold nursing homes accountable for negligence. By doing so, they promote safe living conditions and medical treatment for all nursing home residents.
Secure Expert Legal Representation!
If you or your loved one has suffered from diabetes complications due to nursing home neglect, you are not alone. Our team of experienced and compassionate lawyers at the Nursing Home Law Center is here to help when you are ready to get justice.
Contact us at (800) 926-7565 or complete our online form for a free consultation. We can explain your legal options, recommend legal courses of action, and help you recover compensation for your damages.
References: [1] NIH, [2] Hopkin’s Medicine