The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Carson City Nursing Home Abuse Lawyer
Nursing home abuse is a serious issue that affects countless seniors across Nevada, including Carson City. When families place their loved ones in nursing homes, they trust that these care facilities will provide a safe and respectful environment. Unfortunately, abuse and neglect can occur, leading to physical harm, emotional trauma, and deteriorating health for elderly residents.
For victims and their families, seeking help from an experienced Carson City nursing home abuse lawyer is essential. Legal action not only brings relief to the affected victim but also helps protect other residents from similar harm, making it a critical step toward accountability and improved care standards.
A lawyer can help families explore their legal process, helping to hold responsible parties accountable and ensuring that victims receive the justice and compensation they deserve.
Why Hire Nursing Home Law Center
At Nursing Home Law Center, we fight for justice and fair compensation for nursing home abuse victims. Our experienced Nevada nursing home abuse lawyers have secured substantial settlements and verdicts for clients through years of handling these sensitive cases.
We thoroughly investigate all aspects of abuse—from medical costs to emotional suffering—to build strong cases for our clients. Our deep understanding of nursing home abuse law enables us to navigate legal complexities while vigorously protecting your rights.
We provide clear communication and compassionate support throughout your case, ensuring your family feels informed and protected.
Types of Cases Handled by Our Carson City Nursing Home Abuse Lawyers
Nursing home abuse involves any act or neglect that harms, exploits, or mistreats seniors in care facilities. Abuse can manifest in various forms, impacting the physical, emotional, and financial well-being of residents. Our Carson City elder abuse lawyers handle a wide range of cases, helping families seek legal advocacy for their elderly loved ones.
Physical Abuse
Physical abuse includes any intentional use of force against a resident that results in injury or pain. This bodily assault can involve hitting, slapping, pushing, and improper use of physical restraints.
Mental and Emotional Abuse
Mental and emotional abuse involves actions that cause psychological harm or distress to elderly residents. This type of abuse may not leave physical signs but can have lasting effects. Examples include verbal insults, threats, humiliation, and intentional isolation from others.
Sexual Abuse
Sexual abuse in nursing homes includes any non-consensual sexual contact or behavior directed at a resident. This form of abuse is particularly traumatic, as many patients are unable to defend themselves. Examples include inappropriate touching, sexual assault, or forced nudity.
Medical Malpractice
Medical malpractice occurs when nursing home staff fail to provide proper medical care, leading to harm or deterioration of a resident’s health. Common examples include untreated bedsores, medication errors, and failure to monitor changes in health conditions.
Negligence
Negligence refers to the failure to provide primary care, harming elderly residents. This neglect can include poor hygiene, malnutrition, dehydration, and lack of supervision. Negligence may also lead to elopement, where patients wander away from the facility unsupervised, posing severe risks.
Financial Abuse
Financial abuse involves exploiting a resident’s economic resources for personal gain. This exploitation can include theft, unauthorized access to bank accounts, or coercing the resident to sign over assets.
Wrongful Death
In the most tragic cases, abuse or neglect can lead to the death of a resident. Wrongful death claims arise when a resident dies due to untreated infections, medication errors, or lack of supervision.
Understanding Your Legal Rights
Various federal and state laws protect nursing home patients, ensuring they receive quality care, emotional support, respect, and protection from abuse and neglect.
The Nursing Home Reform Act of 1987 is a significant federal law that protects nursing home residents’ rights. This law, part of the Omnibus Budget Reconciliation Act, sets standards for all nursing homes receiving federal funding through Medicare or Medicaid. The act mandates that nursing homes provide services that enhance residents’ quality of life and preserve their dignity.
In addition to federal protections, Nevada has specific laws and regulations that govern the operation of nursing homes and protect patients from harm.
The Nevada Division of Public and Behavioral Health oversees nursing home licensing, inspections, and enforcement. Nevada law requires that nursing homes provide adequate staffing, maintain a safe and clean environment, and ensure appropriate medical care.
Eligibility to File a Nursing Home Abuse Claim
When a nursing home resident’s rights are violated, they may file a claim directly against the responsible parties for any harm they have suffered. If a resident is incapacitated or unable to act, family members may initiate a claim on their behalf.
If the resident has a designated legal representative, such as a power of attorney or guardian, that person can file the claim on their behalf.
In cases where abuse or neglect caused the resident’s death, the estate’s executor or a family member may pursue a wrongful death claim to seek justice and compensation.
Common Signs of Elder Abuse Among Nursing Home Residents
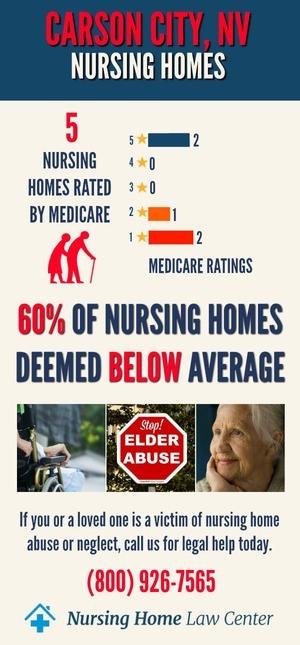
There are 10 Medicare-certified nursing homes in Carson City, and many of these facilities are struggling with their overall ratings and inspections. Specifically, 80% of these homes, or 59.3%, have received an overall rating of below or much below average.
Health inspections are a critical concern, as 80% of facilities scored poorly in this category. These low scores suggest widespread issues related to compliance with state and federal health regulations, potentially affecting residents’ well-being.
Staffing levels also present challenges, with 50% of nursing homes receiving below-average ratings. These staffing deficiencies may reflect difficulties in providing consistent, adequate care for residents, impacting their day-to-day well-being and long-term health.
30% of facilities are rated poorly in quality measures, indicating that nearly a third of facilities still perform reasonably well in maintaining residents’ overall quality of care. [1]
Abuse can take many forms, each causing physical injuries, emotional distress, and financial harm. Often, the identifying signs of abuse are subtle, so it’s important to stay vigilant for indicators of mistreatment.
- Unexplained injuries, such as bruises, cuts, fractures, or burns
- Bedsores (pressure ulcers)
- Sudden weight loss
- Weakness and fatigue
- Dry skin or signs of dehydration
- Sudden or unusual behavioral changes
- Fear of certain staff members
- Poor hygiene or unsanitary living conditions
- Missing valuables
- Sudden changes in financial documents
The worst-rated nursing homes in Carson City include:
| Alta Skilled Nursing and Rehabilitation Center | Carson Nursing and Rehabilitation Center |
| Caremeridian Llc, Dba Neurorestorative | Gardnerville Health & Rehabilitation Center |
| Ormsby Post Acute Rehabilitation |
The Cost of Hiring a Carson City Nursing Home Abuse Attorney
At Nursing Home Law Center, we understand that financial concerns can be a significant barrier for families seeking justice. To make our services accessible, our nursing home abuse and negligence law firm operates on a contingency fee basis. This arrangement means you pay nothing upfront, and our fee is only collected if we secure compensation for you.
You Have Limited Time to Take Legal Action in Carson City
In Nevada, there is a specific time limit, known as the statute of limitations, for filing a nursing home abuse claim. Generally, victims and their families have two years from the date of the incident or the discovery of the abuse to pursue legal action. Missing this deadline can mean losing the right to seek compensation and justice, making it critical to act quickly.
Contact a Carson City Nursing Home Abuse Attorney Today!
At Nursing Home Law Center, our experienced lawyers are dedicated to fighting for justice on behalf of nursing home abuse victims in Carson City. With a proven track record of securing significant settlements and favorable verdicts, our team understands the complex challenges of nursing home abuse cases.
Our law firm works tirelessly to hold responsible parties accountable and to ensure that victims receive fair compensation for their suffering.
If you suspect that your elderly loved one has been a victim of abuse or neglect in a Carson City nursing home, don’t wait. Call us at (800) 926-7565 or fill out our contact form to book a free consultation and explore your legal options.
References: [1] Medicare

