The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Bethesda Nursing Home Abuse Lawyer

Licensed in Maryland
Elder abuse is a serious and growing concern for families who trust nursing homes to provide a safe environment and quality care for their elderly loved ones. Unfortunately, many elderly residents suffer poor treatment, exploitation, or nursing home neglect.
These acts of abuse can cause serious injuries and mental distress and, in severe cases, lead to loss of life. When abuse and neglect occur, it erodes trust and poses significant risks to the health and well-being of residents.
Victims and their families should seek the help of experienced Bethesda nursing home abuse attorneys when abuse occurs. They understand the complexities of these cases, can conduct thorough investigations, and hold responsible parties accountable.
Why Hire Nursing Home Law Center
At Nursing Home Law Center, we are dedicated to securing fair compensation for those affected by nursing home abuse. Our seasoned legal team has a strong history of managing nursing home abuse cases and obtaining substantial settlements and favorable verdicts.
We conduct comprehensive investigations to cover every detail of abuse, addressing medical expenses, emotional trauma, and other related damages. With our extensive knowledge of nursing home abuse claims, we handle the process efficiently and fight relentlessly to protect your rights.
Types of Cases Handled by Our Bethesda Nursing Home Abuse Lawyers
Elder abuse involves any act or failure to act by caregivers or other residents that endangers the well-being of residents in nursing home facilities. This act can include various types of abuse and neglect that compromise the safety, health, and dignity of residents. Below, we outline the primary types of cases our abuse lawyers handle.
Physical Abuse
Physical elderly abuse is any intentional act that causes pain or injury, such as hitting, slapping, or rough handling. It also includes the improper use of restraints, which can lead to physical harm or unexplained injuries like broken bones or bruises.
Mental and Emotional Abuse
Mental and emotional elderly abuse involves actions that cause psychological distress to a nursing home patient, including verbal threats, humiliation, or isolation. This type of abuse can result in depression, anxiety, and a significant decline in mental health.
Sexual Abuse
Sexual abuse includes any non-consensual sexual contact or behavior directed toward a resident. Patients with cognitive impairments fall at risk of this form of abuse as they may be unable to communicate the sexual violation. Indicators may include sudden fear, behavioral shifts, or physical signs like bruising or trauma.
Medical Malpractice
Medical malpractice in nursing homes often results from substandard medical care provided by staff members or health care providers. Common examples include untreated bed sores, medication errors, or failure to respond adequately to medical emergencies.
These lapses can cause serious injuries and, if not treated, can worsen a resident’s condition or lead to severe complications.
Negligence
Negligence involves failing to provide basic care, such as proper hygiene, adequate nutrition, or hydration. Due to neglectful practices, patients may suffer from poor hygiene, malnutrition, or dehydration. Elopement—when residents wander unsupervised and put themselves at risk—is another significant form of nursing home negligence that can lead to severe injuries.
Financial Abuse
Financial abuse refers to the unauthorized or illegal use of a resident’s assets or funds. This exploitation could include forging signatures, stealing money or belongings, or coercing residents into altering financial documents.
Wrongful Death
When nursing home abuse and neglect result in the death of a resident, it may be considered wrongful death. This loss can stem from severe neglect, medical malpractice, or deliberate abuse. A family member or legal representative may pursue a wrongful death claim to hold nursing homes accountable for their failure to prevent abuse and neglect.
Understanding Your Legal Rights
Nursing home residents have protected rights under federal and state laws to ensure their safety, dignity, and quality of life.
One critical federal law is the Nursing Home Reform Act of 1987. It sets strict regulations for nursing home facilities and mandates that residents have access to proper medical care, adequate nutrition, and clean living conditions. This act ensures residents can live free from abuse, neglect, and other forms of mistreatment.
In Maryland, state-specific laws complement federal regulations by enforcing strict licensing and oversight for nursing homes and assisted living facilities. The Maryland Department of Health monitors compliance and conducts inspections to identify and address any violations that could harm residents.
A nursing home abuse claim can be filed by the victim or, if they are unable to act, by a legal guardian or their estate. In cases where abuse and neglect lead to death, surviving family members have the right to file a wrongful death claim.
Seeking legal counsel can help families understand their rights and take appropriate legal action to ensure nursing homes are held accountable for their actions or failures.
Liability in Nursing Home Neglect and Abuse Cases
In nursing home abuse and neglect cases, multiple parties may be liable for the harm caused to residents. Consulting with a skilled Bethesda nursing home lawyer can help victims and families identify liable parties and pursue the justice and financial compensation they deserve. Below are some examples of who may be held liable in these cases:
- Nursing Home Facilities: The nursing home can be liable if poor policies, understaffing, or inadequate training lead to neglect or abuse.
- Nursing Home Administrators and Operators: Administrators and nursing home operators oversee the facility’s day-to-day operations. If they fail to implement safety measures or properly screen and train employees, they may be liable for abuse or neglect.
- Staff Members: Individual staff members can be held accountable for direct acts of abuse. For example, an aide who uses excessive force or intentionally harms a resident can face civil and criminal consequences.
- Medical Professionals: Healthcare providers within nursing homes may be liable for medical negligence if they fail to provide appropriate medical care. This neglect includes errors such as medication mistakes or not addressing issues like bed sores, which can lead to severe complications if not treated.
- Third-Party Contractors: Contractors, such as therapists or maintenance workers, may also be held responsible if their negligence contributes to nursing home injuries. For instance, a contractor who fails to fix safety hazards that result in resident falls or injuries could be deemed liable.
How Our Bethesda Nursing Home Abuse Attorneys Can Help
Our Maryland nursing home neglect attorneys are dedicated to ensuring elderly residents receive the justice and financial compensation they deserve for the harm they have suffered.
Our law firm has successfully handled numerous nursing home abuse and neglect cases, providing compassionate, effective representation to clients throughout Montgomery County and beyond.
Below are the services we offer to support victims and their families:
Free Case Evaluation
We start by offering a free consultation to assess your case. This initial evaluation allows our legal team to review the case details, determine the strength of your claim, and provide guidance on your next steps without any financial risk to you.
Case Investigation
Our lawyers conduct thorough investigations to gather all necessary evidence, including medical records, witness statements, and facility inspection reports. This comprehensive approach ensures that we can build a strong case to show how the nursing home facility failed to provide quality care and contributed to the resident’s suffering.
Filing the Claim
We handle all aspects of the legal process for filing your claim, including preparing and submitting the required documents under Maryland regulations. By managing this process, we help alleviate the stress on you and your family while ensuring that your claim is filed accurately and on time.
Settlement Negotiation
Our lawyers are skilled negotiators who will pursue fair settlements that reflect the full scope of your damages. We work directly with the insurance company and opposing counsel to achieve a favorable resolution for you and your elderly loved one.
Trial Representation
Our team is prepared to take your case to trial if a fair settlement cannot be reached. With a history of successful verdicts, we provide robust representation to ensure those responsible are held accountable for their actions.
Common Signs of Elder Abuse Among Nursing Home Residents
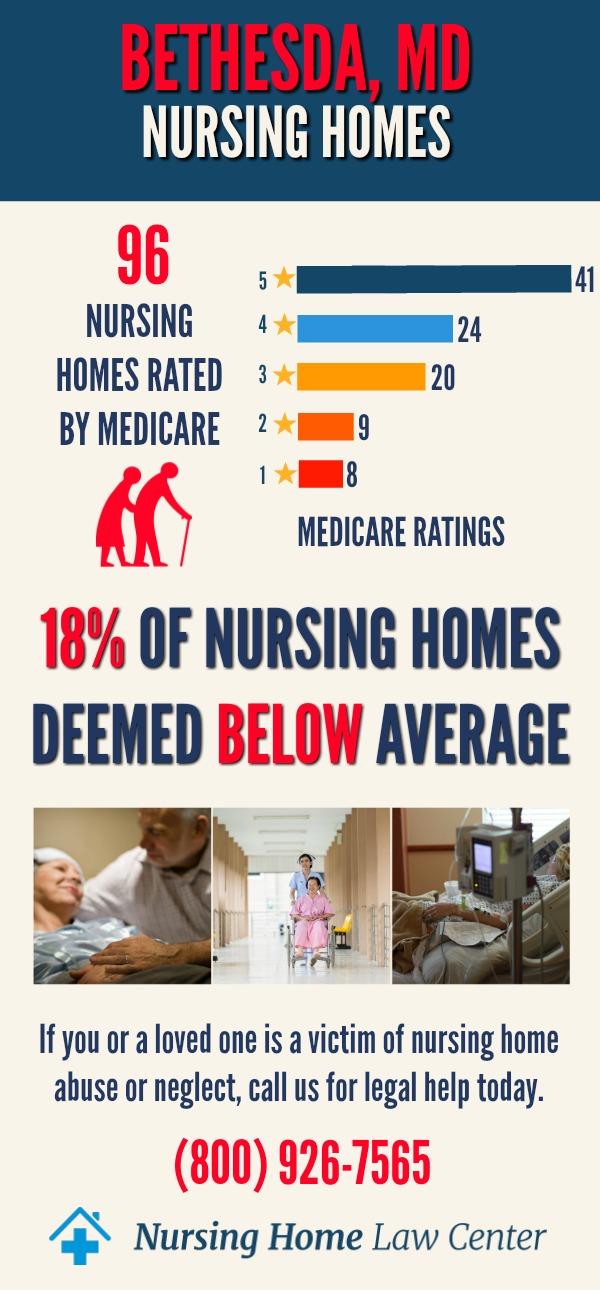
There are 104 Medicare-approved nursing homes in Bethesda, MD. Thirty-four (33%) have an overall score rated below or much below average, indicating that a third of facilities fall short in overall quality.
The situation is similarly troubling in health inspections, where 38 nursing homes (37%) have below-average scores, reflecting issues in compliance with health and safety standards.
Staffing levels present another challenge, with 32 facilities (31%) rated poorly, suggesting potential inadequacies in caregiver availability and resident support.
Quality measures, which assess how well residents’ needs are met, are the most promising area, with only 14 nursing homes (approximately 13%) scoring below average. [1]
Recognizing the signs of abuse is critical to protecting elderly loved ones residing in nursing facilities.
- Unexplained Injuries: Watch for bruises, cuts, or burns that nursing home staff cannot explain. Recurring or multiple injuries in various stages of healing may point to ongoing physical assault.
- Signs of Restraints: Marks on the wrists, ankles, or other body parts may suggest the improper or excessive use of physical restraints.
- Sudden Mood Changes: Psychological abuse can cause noticeable mood shifts, including heightened anxiety, depression, or sudden withdrawal from social activities and interactions.
- Fear of Staff Members: A resident who shows signs of anxiety, avoids eye contact, or appears anxious around a specific staff member could be reacting to abuse or intimidation.
- Unexplained Genital Injuries: Any injuries or infections in the genital region should be taken seriously and investigated, as they may indicate sexual assault.
- Untreated Bedsores: Bedsores (pressure ulcers) are a clear sign of neglect. If left untreated, they can become infected, resulting in severe health issues for the residents.
- Malnutrition or Dehydration: Signs like significant weight loss, dry skin, or general weakness could indicate that the resident is not receiving adequate nutrition or hydration, pointing to nursing home neglect.
- Unexplained Financial Activity: Sudden and suspicious financial changes, such as large or unexplained withdrawals, missing belongings, or unauthorized modifications to wills or financial documents, may indicate financial exploitation.
- Withdrawal from Social Activities: A formerly sociable resident who becomes withdrawn or refuses to engage in activities may be experiencing psychological abuse or deliberate isolation by a staff member.
Families must stay vigilant for these signs and take swift legal action if they suspect their elderly loved one is being abused or neglected. Consulting a Bethesda nursing home lawyer can help families navigate the legal process and take the steps needed to ensure the safety and rights of their loved ones and other residents.
The worst-rated nursing homes in Bethesda include:
| Adelphi Nursing and Rehabilitation Center | Autumn Lake Healthcare at Arcola |
| Bridgepoint Sub-Acute & Rehab National Harborside | Capitol City Rehab and Healthcare Center |
| Carlin Springs Health & Rehabilitation | Clinton Healthcare Center |
| Fox Chase Healthcare | Largo Nursing and Rehabiliation Center |
| White Oak Rehabilitation and Nursing Center |
What to Do If You Suspect Nursing Home Abuse
If you believe that an elderly loved one is experiencing nursing home abuse, it is essential to act quickly to protect them. Here are the recommended steps to take:
- Call 911 if Immediate Danger is Present: If you suspect the resident is at immediate risk of harm, contact 911 to ensure they receive prompt attention from emergency services and law enforcement.
- Report to the Nursing Home Administrator or Management: Notify the nursing home administrators or facility management of your concerns. This report can trigger an internal investigation and prompt immediate action to protect the resident.
- File a Complaint with your Local Ombudsman’s Office: The Ombudsman’s office advocates for residents in nursing homes and assisted living facilities. They help investigate complaints, mediate issues, and work to resolve problems related to resident care. Filing a complaint with them can ensure an independent review of the situation.
- Contact a Nursing Home Abuse Lawyer: Contact an experienced nursing home attorney in Bethesda, MD, for legal guidance. A lawyer can help you understand your rights, collect evidence, and take the necessary steps to pursue a nursing home abuse claim. They will support you through the legal process to seek justice and ensure those responsible are held accountable.
Damages You Can Recover Through a Nursing Home Abuse Claim
Victims of nursing home abuse and their family members can seek various types of damages to compensate for the harm suffered. Below are the primary categories of damages that can be pursued in a nursing home abuse claim:
Economic Damages
These damages cover the tangible costs associated with abuse or nursing home negligence:
- Medical expenses: Reimbursement for costs related to hospital stays, treatment, medications, and rehabilitation.
- Relocation costs: Expenses incurred when moving the resident to a safer nursing home or care facility.
- Lost assets: Compensation for financial losses from abuse, such as stolen money or valuables.
Non-Economic Damages
Non-economic damages provide compensation for the emotional and psychological toll of the abuse:
- Pain and suffering: Monetary compensation for the physical pain and discomfort endured by the resident.
- Emotional distress: Damages for the mental trauma caused by abuse or neglect.
- Loss of enjoyment of life: Compensation when the resident’s quality of life is reduced due to the abuse.
Punitive Damages
Punitive damages may be awarded when the abuse was reckless or intentional. These damages are designed to punish the responsible nursing home or individuals and deter similar conduct in the future.
Wrongful Death Damages
If nursing home abuse and neglect result in the death of a resident, surviving family members can file a wrongful death claim. Compensation in these cases may include:
- Funeral and burial expenses: Coverage for the costs of end-of-life services.
- Loss of companionship: Damages for the emotional loss experienced by the family due to the death of their loved one.
- Loss of financial support: Compensation for the economic contributions the deceased would have provided to their dependents.
These damages help families recover from the emotional and financial impacts of the abuse or neglect and ensure the nursing home is held accountable for its actions. Consulting with a skilled Bethesda, MD, nursing home neglect attorney can guide you in understanding what damages you may be entitled to and how to pursue them effectively.
The Cost of Hiring a Bethesda Nursing Home Abuse Lawyer
At our law firm, we understand that the financial burden of seeking legal representation can be a concern for families. To make justice accessible, we operate on a contingency fee basis for nursing home abuse cases.
This arrangement means you do not pay any upfront fees or out-of-pocket costs. We only collect our fee if we successfully recover your financial compensation through a settlement or verdict.
This approach ensures that families can pursue their nursing home abuse claim without worrying about legal expenses, allowing them to focus on supporting their loved ones.
You Have Limited Time to Take Legal Action in Bethesda
If you suspect that your elderly loved one is being abused in a Bethesda nursing facility, it’s crucial to act swiftly due to Maryland’s statute of limitations.
In most cases, the law allows three years from the date of the incident or the discovery of the abuse to file a claim. However, certain situations, such as cases involving incapacitated residents or wrongful death, may impact the timeline.
Missing this deadline can mean losing the opportunity to seek financial compensation and hold the nursing home accountable. Consulting an experienced Bethesda, MD, nursing home neglect attorney as soon as possible helps ensure your case is filed within the allowable period, preserving your rights and maximizing the potential for a successful outcome.
Contact a Bethesda Nursing Home Abuse Attorney Today!
Our law firm has extensive experience representing victims of nursing home abuse and neglect in Bethesda and throughout Montgomery County.
We are committed to holding nursing homes and their staff accountable and have a proven track record of securing financial compensation for our clients. Our dedicated team offers compassionate guidance and effective legal strategies to support you and your elderly loved one through every step of the process.
If you suspect that a loved one is being abused in a nursing home facility, don’t wait to seek help. Contact us for a free consultation to discuss your case and explore your legal options.
Call us at (800) 926-7565 or fill out our contact form.
References: [1] Medicare
Maryland Nursing Home Abuse Lawyers
Maryland nursing home abuse lawyers are dedicated to seeking justice for families throughout the state. From Baltimore to Bowie, Columbia, MD, Frederick, Gaithersburg, Germantown, Hagerstown, Rockville, Silver Spring, and Towson, our experienced legal team is ready to hold negligent nursing homes accountable. Contact a lawyer in Maryland today to discuss how we can help you fight for your loved one’s rights and ensure they receive the care they deserve.