legal resources necessary to hold negligent facilities accountable.
St. Louis Nursing Home Abuse Lawyer
 Incidents of neglect and abuse in nursing homes not only cause immediate harm to residents but also have long-term effects on their health and well-being. The extent of this issue underscores the need for vigilant monitoring and accountability in elder care facilities.
Incidents of neglect and abuse in nursing homes not only cause immediate harm to residents but also have long-term effects on their health and well-being. The extent of this issue underscores the need for vigilant monitoring and accountability in elder care facilities.
At Nursing Home Law Center, LLC, our nursing home abuse lawyer focuses on representing victims and their families in these distressing situations. We aim to deliver justice and promote safer environments for all nursing home residents.
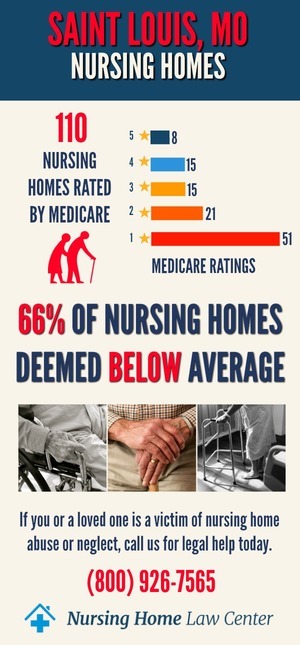
Nursing Home Statistics in St. Louis, MissouriThe Centers for Medicare and Medicaid Services (CMS) January 2024 updated findings revealed concerning statistics regarding St. Louis, Missouri nursing homes. Out of the 128 facilities assessed, a staggering 88, constituting 69% of the total, received ratings categorized as "below average" or "much below average." This alarming trend raises significant concerns about the quality of care these nursing facilities provide.
Furthermore, inspectors have cited several facilities for instances of abuse, highlighting the need for comprehensive investigations and intervention to protect elder care home patients. The following facilities have been cited for abuse:
- Amberwood Estates Nursing and Rehabilitation
- Aspen Point Health and Rehabilitation
- Athene Nursing and Rehabilitation
- Bellefontaine Gardens Nursing & Rehab
- Bethesda Dilworth
- Bria of Alton
- Bria of Cahokia
- Caseyville Nursing & Rehab Center
- Chestnut Rehab and Nursing
- Crestwood Health Care Center
- Delmar Gardens West
- Edwardsville Nsg & Rehab Center
- Elmwood Nursing & Rehab Center
- Estates of Spanish Lake
- Green Park Senior Living Community
- Life Care Center of Bridgeton
- Manchester Rehab and Healthcare Center
- Mary, Queen, and Mother Center
- Mercy Rehab and Care Center
- Normandy Nursing Center
- Quarters at Des Peres
- St Peters Manor Care Center
- Stearns Nursing & Rehab Center
- Westchester House
The prevalence of nursing home abuse in these facilities underscores the importance of vigilance, advocacy, and taking legal action to protect resident rights.
Why CMS and State Agencies Inspect Nursing HomesCMS and state agencies routinely inspect nursing facilities annually and send investigators to facilities after abused or neglected victims and their families file formal complaints for several crucial reasons:
- Ensuring Quality Care: Annual inspections and investigations help ensure that nursing homes provide their residents with the highest standard of care.
- Protecting Vulnerable Residents: These actions are essential to protect the rights and safety of nursing home residents, especially those who may be victims of abuse or neglect.
- Accountability: Inspections and investigations hold nursing home facilities accountable for alleged abuse or neglect, ensuring they adhere to state and federal regulations.
- Legal Recourse: It provides a foundation for nursing facility abuse attorneys and lawyers to build personal injury claims or wrongful death claims on behalf of the victims and their families.
By monitoring elder care home facilities and responding to complaints, CMS and state agencies play a crucial role in upholding the rights and well-being of elderly residents and those in need of care.
If you suspect nursing home abuse, it's crucial to seek legal guidance for a free case evaluation and explore your options for obtaining justice and financial compensation for your loved one's injuries or losses. Don't hesitate to contact experienced nursing home abuse attorneys who can advocate for you in your nursing home abuse case.
Recognizing Signs of Mistreatment: Different Forms of Nursing Home AbuseThe well-being and safety of residents are paramount in nursing and assisted living facilities. However, there are unfortunate instances where nursing home residents fall victim to various forms of mistreatment. Such mistreatment, whether at the hands of nursing home staff or other residents, can lead to severe harm or even the untimely demise of these vulnerable individuals.
This reality underscores the critical importance of vigilance and awareness in detecting and addressing any signs of abuse or neglect. To assist in identifying and understanding these forms of mistreatment, consider the following key indicators:
- Physical Abuse: This involves injuries like bruises, cuts, or broken bones, often lacking a clear explanation or receiving inconsistent accounts from staff members. Such unexplained injuries are red flags for potential abuse within the nursing home facility.
- Emotional Abuse: This type of abuse is evident through signs of depression, withdrawal, or fear in residents, especially noticeable in the presence of particular staff members or fellow residents. These signs can indicate ongoing emotional distress caused by abusive interactions.
- Sexual Abuse: Indications of sexual abuse include non-consensual sexual contact, evidenced by physical signs or sudden behavioral changes. Any sexual assault is a severe violation, demanding immediate investigation and intervention.
- Financial Abuse: Unexplained financial transactions, such as withdrawals from bank accounts, alterations in wills, or missing personal belongings, can signal financial exploitation of a resident. This form of abuse often goes unnoticed and can lead to significant financial losses for the victim.
- Neglect: Signs of nursing home neglect are apparent through poor hygiene, malnutrition, the development of pressure ulcers (bed sores), or untreated medical conditions. Such neglect reflects the nursing home staff's lack of medical attention and care.
- Medical Malpractice includes instances where the medical treatment provided by the nursing home falls below the standard of care, leading to harm or exacerbation of conditions in the resident.
- Abandonment and isolation occur when a nursing home resident is left without necessary support, interaction, or care, leading to physical and emotional trauma.
Recognizing these warning signs is the first step in protecting residents from abuse and neglect. It's vital for family members and loved ones to remain vigilant and seek a free and confidential consultation with a nursing home abuse attorney if they suspect nursing home neglect or abuse.
A nursing facility abuse lawsuit can not only help recover compensation for medical expenses and emotional distress caused but also ensure that such negligent facilities are held accountable for their actions.
Identifying Abuse and Neglect in Nursing HomesAbuse and neglect in nursing homes can take many forms. Physical abuse includes any act that causes physical harm, such as hitting, pushing, or inappropriate use of restraints. Emotional abuse, though less visible, is equally harmful and includes actions like intimidation, humiliation, or isolation. Financial exploitation, a growing concern, involves the illegal or unauthorized use of an elderly person's assets.
Neglect is another form of abuse characterized by the failure to provide necessary care. This can result in poor personal hygiene, malnutrition, and unattended medical needs. In many cases, neglect arises from inadequate staffing or insufficient training of nursing home staff members. Recognizing these signs is vital in protecting the health and dignity of nursing home residents.
In instances of suspected abuse or neglect, our nursing home neglect lawyers are prepared to take swift action. We work to ensure that victims receive the necessary medical care and support while pursuing legal avenues to hold the responsible parties accountable. Our goal is to provide a voice for those who cannot speak for themselves and seek justice on their behalf.
Immediate Actions to TakeWhen abuse is suspected, immediate action is necessary to protect the victim and preserve evidence.
- The first step is to ensure the safety of the nursing home resident. This may involve relocating them to a safe environment or ensuring they receive immediate medical attention for injuries sustained.
- Reporting the abuse to the authorities is a critical next step. This includes contacting the Missouri Department of Senior Services or local law enforcement. Our law firm assists in making these reports, ensuring they are thorough and effective.
- Documenting evidence of the abuse, such as taking photographs of injuries and preserving any relevant documentation, is critical to pursuing a legal avenue.
- Legal guidance is crucial in navigating the complexities of nursing home abuse lawsuits. Family members should also consider scheduling a free consultation with a nursing facility abuse lawyer.
Our attorneys offer free and confidential consultations to discuss the case's specifics, outline legal options, and plan the next steps in seeking justice and compensation for the victim.
Understanding the Legal Landscape of Nursing Home AbuseThe legal landscape of nursing facility abuse in St. Louis involves state and federal regulations. As experienced nursing facility abuse attorneys, we deeply understand these laws and how they apply to individual cases. This knowledge is crucial in building solid legal cases against negligent facilities and individuals.
Nursing home abuse cases often involve a combination of personal injury law, elder law, and medical malpractice statutes. Our legal team is skilled in navigating these areas, ensuring that all legal aspects of a case are thoroughly addressed. We work tirelessly to ensure that victims' rights are upheld and that they receive the justice they deserve.
A significant aspect of these cases is proving negligence or intentional harm. This requires a detailed investigation and evidence gathering, such as medical records, staff logs, and witness statements.
Recognizing and Responding to Nursing Home Abuse in St. LouisIn St. Louis, recognizing and responding to nursing facility abuse is a critical concern for elderly nursing home residents and their families. Abuse in these facilities can manifest in various forms, each detrimental to the well-being and dignity of residents.
Our nursing home neglect lawyers understand the importance of identifying abuse early and taking decisive action to address it. Our commitment is to ensure that victims receive the care, respect, and justice they deserve.
Investigating and Reporting Nursing Home Neglect and AbuseThe first step in combating nursing facility abuse is recognizing its signs. These can range from physical injuries to subtle changes in behavior that indicate emotional or psychological harm. Each nursing home abuse attorney on our legal team is trained to identify these signs and understand their implications. We work closely with families and medical professionals to ensure that every instance of suspected abuse is thoroughly investigated.
Once nursing home neglect or abuse is identified, immediate action is essential. This includes reporting the incident to the appropriate authorities, such as the Missouri Department of Senior Services or law enforcement. We also work with nursing home administrators and staff to address the immediate safety concerns of the residents and prevent further harm.
The Imperative of Reporting Nursing Home Abuse: a Guide for Kansas City ResidentsEnsuring the safety and well-being of residents in nursing homes is a matter of utmost concern. Reporting any form of nursing home neglect or abuse is not just a moral obligation but a crucial action that can safeguard the vulnerable and hold negligent parties accountable.
When neglect or abuse in nursing facilities goes unreported, it not only continues the cycle of harm to residents but also allows irresponsible facilities and staff to evade legal responsibility.
Where to File a Formal Complaint in Kansas CityIf you are in St. Louis and need to report abuse or neglect in a nursing home, there are several avenues to consider:
- Local Health Department: Contacting the local health department is a primary step. They can initiate investigations into health and safety violations at caregiving homes.
- Missouri Health and Human Services Department: The state department responsible for health and human services can receive complaints regarding nursing home facilities. They can investigate and enforce regulations involving nursing home neglect and abuse.
- Adult Protective Services (APS): APS is responsible for assisting vulnerable adults who are victims of abuse, neglect, or exploitation. They can be contacted to report any form of mistreatment of elderly residents.
- St. Louis Ombudsman Program: The Ombudsman program advocates for residents' rights in long-term care facilities. They can help address complaints about the quality of care or treatment in nursing facilities.
- State Licensing Agency: Reporting to the agency responsible for licensing nursing homes in Kansas City can prompt an investigation into license violations and enforce corrective measures.
- Local Law Enforcement: If immediate danger or criminal activity is suspected, contacting local law enforcement at 911 is necessary.
Remember, reporting nursing home abuse is a critical step toward ensuring the safety of elderly and vulnerable individuals. Your actions can bring about positive change and ensure that nursing facilities provide the care and respect their residents deserve.
Understanding the Legal Landscape of Nursing Home AbuseThe legal landscape of elder abuse encompasses various laws and regulations to protect nursing home patients. These laws provide a framework for addressing instances of nursing home negligence and hold facilities accountable for their actions. As experienced St Louis nursing home abuse lawyers, our firm is well-versed in these regulations. It employs them to defend the rights of the elderly and seek financial compensation for the harm they've endured.
Missouri law requires that nursing homes provide a standard of care that ensures the safety and well-being of their residents. When a nursing home facility fails to meet these standards, resulting in harm to a resident, it constitutes negligence. Our lawyers can assess the situation and determine if there is a viable personal injury case or wrongful death claim.
In instances of elder abuse or sexual abuse, it is not only the direct perpetrator who may be held liable. The nursing home industry at large can be accountable, mainly if systemic issues within a St. Louis nursing or assisted living facility allow the abuse to occur.
Our nursing home abuse lawyers have the expertise to navigate these complex cases, ensuring that both direct and indirect contributors to abuse are brought to justice.
Missouri Statute of LimitationsThe Missouri Statute of Limitations sets a legal time limit for filing nursing facility abuse and neglect claims. This period is crucial as it dictates the window within which a family member can file a lawsuit on behalf of their elderly person. Understanding these time constraints is vital, and our St Louis nursing home abuse lawyer team ensures that all necessary legal actions are taken promptly.
This statute is designed to encourage timely reporting and resolution of abuse cases. However, it can also pose a challenge for families who may only uncover evidence of abuse or neglect after a significant period has passed. Our abuse lawyers provide a detailed explanation during a confidential and free case evaluation, helping clients understand their rights and the urgency required in these legal matters.
Delaying action can result in the loss of the right to recover compensation, including:
- Medical treatment
- Personal property damage
- Other losses related to the abuse
Immediate consultation with a neglect lawyer is imperative. The United States Department of Health and Human Services emphasizes the importance of quick action, and our firm aligns with this guidance, providing swift and decisive legal support.
The Role of an Experienced St Louis Nursing Home Abuse LawyerThe role of experienced nursing home abuse attorneys is pivotal when a nursing home resident falls victim to abuse or neglect. These legal professionals are the advocates for the injured and their family members, navigating the complex legalities of St Louis nursing home abuse cases. A free consultation with our firm can start the process of a personal injury case, where the goal is to address the nursing facility negligence that has caused so much pain and suffering.
Our nursing home lawyers specialize in dissecting the nuances of each case, understanding that the symptoms of abuse, such as pressure ulcers or emotional withdrawal, are often hidden or misconstrued. The expertise we bring to the table is invaluable in recognizing the common signs of abuse and building a solid case to present in court. This expertise extends to navigating the specifics of St Louis nursing home regulations and care standards.
When neglect victims come forward, it is often due to the diligence of staff members who witness elder abuse and take a stand. Our firm collaborates with these conscientious individuals, using their testimony and the evidence they provide to strengthen the case against a negligent facility.
The facility manager and their insurance company may attempt to dispute claims. Still, our seasoned attorneys are well-equipped to counter these tactics and advocate for the rights of the abused.
Legal Representation and AdvocacyLegal representation and advocacy are about more than just navigating court proceedings; they're about ensuring justice for the adult abuse victim and holding the responsible parties accountable. Our St Louis nursing home abuse attorneys are staunch advocates for the elderly and their rights. We understand that a successful claim can help secure the medical care and financial resources necessary for victims to recover and live with dignity.
Choosing the proper legal representation is critical for the victim and their family. Our St Louis nursing home lawyers understand the unique circumstances of each case, offering a personalized approach to legal advocacy. We work tirelessly to ensure that every nursing home resident receives the attention and legal support they deserve in the face of abuse.
Our advocacy doesn't end in the courtroom. We also strive to raise awareness about elder abuse, educate nursing home staff members, and push for stricter enforcement of care standards. Our efforts aim to win cases and create a safer environment for all St Louis nursing home residents and beyond.
Choosing the Right Law FirmSelecting the right law firm for a nursing facility abuse case is a decision that can significantly impact the outcome for a family member seeking justice. A firm with a strong track record in handling these sensitive cases can offer reassurance that the matter will be addressed with the utmost care and legal acumen. Our St Louis nursing home abuse lawyers have years of experience and a history of success in representing neglect victims and their families.
Our law firm's commitment to victims of nursing home negligence goes beyond the courtroom. We offer comprehensive support, from assisting with insurance company negotiations to helping arrange the best possible medical care. By choosing our firm, clients can rest assured that their case is in the hands of dedicated professionals committed to securing the best possible outcome.
Hire Our St. Louis Nursing Home Abuse Law Firm to Resolve Your Compensation ClaimFacing abusive behavior or negligence can be overwhelming, but you are not alone. Nursing Home Law Center, LLC can help. Call our nursing home abuse lawyers at (800) 926-7565 for a free consultation.
We accept all cases on a contingency fee arrangement, meaning you don't pay any upfront fees until we win your case.
 City of St. Louis Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
City of St. Louis Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
