legal resources necessary to hold negligent facilities accountable.
Schaumburg Nursing Home Abuse Lawyer
 Unfortunately, nursing home abuse is too common and can have devastating consequences for victims. Many cases go unreported because victims might hesitate to speak out about the abuse they suffer for fear of retaliation or further mistreatment.
Unfortunately, nursing home abuse is too common and can have devastating consequences for victims. Many cases go unreported because victims might hesitate to speak out about the abuse they suffer for fear of retaliation or further mistreatment.
Nursing home abuse can lead to serious physical injuries, including broken bones, bed sores, and even death. The emotional effects of abuse can be just as damaging and include depression, anxiety, and post-traumatic stress disorder.
Are you a victim of nursing home neglect, abuse, or mistreatment? If so, the affiliate Illinois personal injury attorneys at Nursing Home Law Center, LLC, can protect your rights.
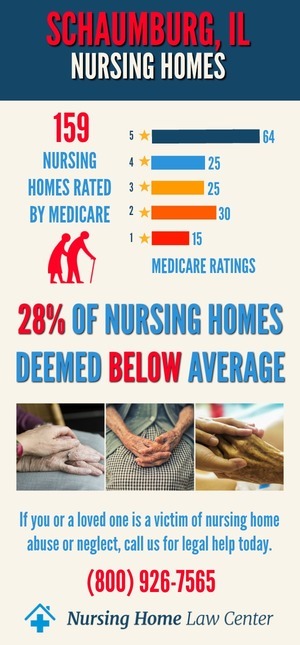
Call our Schaumburg nursing home lawyers at (800) 926-7565 (toll-free phone number) for immediate legal advice and schedule a free consultation. All confidential or sensitive information you share with our legal team remains private through an attorney-client relationship.
What Are Elderly Abuse and Neglect?According to the National Center on Elder Abuse, abusing the elderly involves "a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person."
The Illinois Elder Abuse and Neglect Act defines abuse against the elderly as "the infliction upon an elderly person or disabled adult by a caregiver of physical pain or injury, exploitation, sexual abuse, mental suffering or willful deprivation."
Neglect is the failure of “a caregiver to provide the goods and services necessary to maintain the physical and mental health of an elderly person or disabled adult."
Who Are Most Likely to Abuse, Mistreat, and Neglect the Elderly and Disabled?According to the Illinois Department of Public Health (IDPH), there were 1,872 substantiated cases of abuse in nursing homes across Illinois in 2017. Of those cases, 579 resulted in physical injury to nursing home residents, while 1,293 resulted in emotional harm.
Most abusers are caregivers or family members. In Illinois, the most common type of abuse reported was neglect, followed by psychological abuse and illegal meddling in the patient’s financial affairs.
Do you believe that you or a loved one is a victim of nursing home negligence or abuse? Contact an experienced Schaumburg personal injury lawyer at our law offices as soon as possible.
The State's Nursing Home Abuse and Neglect ActThe Illinois Nursing Home Abuse and Neglect Act provides protections for victims of abuse and their families. Under the Act, neglect, and abuse victims can file a civil lawsuit against the abuser or the nursing facility.
In some Schaumburg nursing home abuse cases, victims might be entitled to compensatory damages, including medical expenses, pain and suffering, and emotional distress. In some nursing abuse cases, punitive damages might also be available.
Mistreating the Elderly and Disabled: A Serious Health Problem in Illinois Nursing HomesThe Centers for Medicare and Medicaid Services (CMS) reports that more than 1 in 10 adults aged 60 years or older have experienced some form of abuse. However, only one in 14 cases of abuse is reported to authorities.
Nursing abuse is a serious problem in nursing facilities across the United States. In Illinois, the Illinois Department of Public Health (IDPH) is responsible for investigating complaints and incidents of abuse, mistreatment, and neglect in nursing homes and assisted living facilities.
Among the disabled residing in nursing facilities and group homes in Illinois, nearly 25 percent will experience nursing home negligence or abuse during their lifetime.
According to a study conducted by the University of Illinois at Urbana-Champaign, disabled adults who live in nursing facilities are nearly three times more likely to be abused than those who do not live in nursing homes.
Signs of Abuse, Mistreatment, and Neglect in Nursing Homes and Assisted Living FacilitiesThe signs of abuse, mistreatment, and neglect can vary depending on the type of mistreatment. However, some general signs might indicate that a nursing home resident is abused or neglected.
If you notice any of the following signs, it might be an indication that the resident is being abused or neglected:
- Unexplained bruises, cuts, or welts
- Broken bones or fractures
- Sprains or dislocations
- Internal bleeding
- Bedsores or pressure ulcers
- Signs of restraint, such as rope marks on wrists or ankles
- Weight loss or gain
- Dehydration or malnourishment
- Unusual mood swings or behavior changes
- Anxiety, depression, or withdrawal from social activities
Physical abuse is the most common form of mistreatment in Illinois nursing facilities. Any forcible harm against nursing home residents might include:
- Hitting and slapping
- Biting
- Shoving
- Pinching
- Burning
- Unauthorized physical or chemical restraints
Sexual abuse could involve unwanted sexual contact or activity, such as rape, sodomy, oral sex, forcing someone to watch sex acts or sexual assault. The abuse can also include unwanted touching, groping, or forced nudity.
Emotional abuse might involve yelling, threats, name-calling, and ridiculing. It can also include isolating disabled patients or elderly senior citizens from friends and family or ignoring a resident's needs.
Financial abuse could involve a caregiver, visitor, family member, friend, or another patient stealing a resident's money or property, forging a resident's signature, or coercing a person to sign financial documents.
Who Can Be Held Liable for Nursing Home Neglect or Abuse?The nursing home, its staff members, or outside health care providers providing services in the nursing home or assisted living facility could be liable for nursing home neglect.
In some cases, the facility itself may be found negligent if it failed to properly screen and train employees or if it was aware of abuse or neglect and failed to take appropriate action.
Anyone including the facility, staff, employees, contracted workers, family members, friends, visitors, other nursing home residents, and others could be liable for abusing a patient at the nursing home facility.
Nursing home neglect cases can be complex, and you must speak with an experienced Illinois nursing home injury lawyer to discuss your legal options.
Hire Nursing Home Abuse Attorneys to Resolve Your Compensation ClaimDo you suspect a loved one is a victim of nursing home negligence or abuse? Act immediately to stop the mistreatment now. An experienced Schaumburg nursing home abuse lawyer from our law offices can review your case, discuss your legal options, and help you get the justice and compensation you deserve.
In some cases, you may be entitled to compensatory damages, including medical expenses, pain and suffering, and emotional distress.
Our affiliate Schaumburg, nursing home abuse lawyers, provide immediate legal representation to injured victims who suffered abuse, mistreatment, or neglect. We currently serve clients throughout the Chicago metropolitan area, including Lake County, Cook County, DuPage County, and Will County.
Contact a nursing home abuse attorney from our law offices today at (800) 926-7565 or use the contact form to schedule a free consultation. Chicago personal injury lawyers are standing by to talk about your legal situation.
Our personal injury lawyers operate on a contingency fee basis, so you don't have to pay us unless we win your case.
Resources: Chicago Attorney Nursing Home Law Center LLC Home
Chicago Attorney Nursing Home Law Center LLC Home
