legal resources necessary to hold negligent facilities accountable.
San Bernardino Nursing Home Abuse Lawyer
 The neglect of nursing home residents often results in critical medical conditions being overlooked, leading to a decline in health and well-being. This form of neglect can manifest in bedsores, malnutrition, or inadequate medical treatment, exacerbating existing health issues.
The neglect of nursing home residents often results in critical medical conditions being overlooked, leading to a decline in health and well-being. This form of neglect can manifest in bedsores, malnutrition, or inadequate medical treatment, exacerbating existing health issues.
The team of nursing home abuse attorneys at Nursing Home Law Center, LLC focuses on these neglect cases, striving to secure the necessary medical care and compensation for affected residents and their families. We are profoundly committed to protecting the rights of whistleblowers, ensuring their safety, and providing robust legal support to bring abusers to justice.
Prevalence of San Bernardino County Nursing Home AbuseAbusing the elderly and disabled in San Bernardino County is a pressing concern, with numerous incidents reported annually. This alarming trend underscores the vulnerability of patients in various care facilities. Addressing this issue requires a comprehensive understanding of this region's scale and nature of abuse.
In San Bernardino County, the growing number of elder abuse cases in assisted living and nursing facilities reflects broader systemic issues. A rise in Bernardino County nursing home abuse cases can be attributed to the following:
- Inadequate staffing
- Lack of proper training
- Insufficient oversight
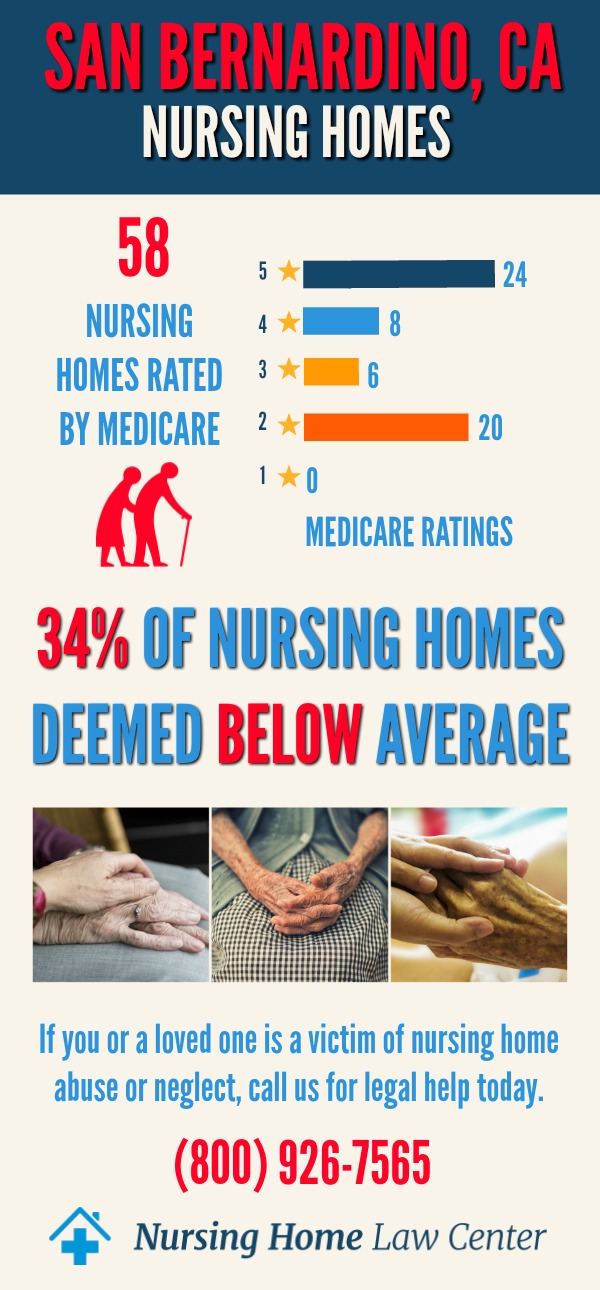
In December 2023, the Centers for Medicare and Medicaid Services (CMS) published a revealing report on the quality of senior care homes in San Bernardino County, California. This report highlights a concerning trend, with a substantial number of these facilities receiving ratings of "below average" or "much below average." Among the 78 assessed San Bernardino County nursing home facilities, 19 (24%) have received these troubling ratings.
Significance of Below-Average RatingsWhen care homes are rated as "below average" or "much below average" by CMS, it raises significant concerns about patient care quality. These ratings indicate issues that can negatively impact the well-being of those residing in these facilities, including:
- Safety
- Staffing
- Cleanliness
- The overall quality of care
Families and individuals considering nursing home care for their loved ones must pay close attention to these statistics.
The statistics and reports from San Bernardino County care facilities reveal a disturbing pattern of nursing home neglect and mistreatment. The high incidence of abuse calls for a concerted effort from legal entities, healthcare providers, and the community.
Protecting Patients in San Bernardino County Nursing Home FacilitiesSan Bernardino's caregiving homes collectively house many patients, making their safety and well-being a paramount concern. These facilities vary in size and the level of care provided, but all are subject to state regulations to safeguard residents. Despite regulations, many facilities struggle with challenges that can lead to nursing home neglect and abuse.
The number of caregiving homes in San Bernardino County continues to grow, reflecting the increasing demand for elder care. However, this expansion must be matched with a commitment to quality care and strict adherence to safety standards.
Common Types of Elder Abuse in Nursing FacilitiesAbusive behavior takes various forms, each with its own set of devastating effects on patients. Recognizing these types is key to prevention and intervention. Below is a comprehensive list of elderly abuse types commonly reported in nursing homes:
- Physical Abuse: Involves acts of violence and rough treatment that cause physical harm to patients.
- Sexual abuse: Encompasses non-consensual sexual contact or exploitation of patients.
- Psychological abuse: Includes verbal assaults, intimidation, or other forms of emotional manipulation that harm the mental well-being of patients.
- Neglect: Occurs when essential care, such as hygiene, nutrition, or medical needs, is not provided, leading to the deterioration of a resident's health.
- Financial abuse: Entails unauthorized or illegal use of a resident's financial resources or coercion for financial gain.
- Resident-to-resident abuse: Involves aggression or mistreatment between senior care home or assisted living facility patients, often due to insufficient supervision.
- Medical malpractice: Refers to substandard care, facility-acquired pressure ulcers (bed sores), or treatment errors that result in injury, worsening condition, or wrongful death.
Identifying these abuse types in a senior care center or assisted living facility helps in taking appropriate actions to protect the patients and hold the perpetrators accountable.
Identifying Signs of Abuse and NeglectRecognizing abuse and neglect in senior care homes is crucial for the timely intervention and protection of residents. Awareness of these signs enables caregivers and family members to take appropriate action, ensuring the safety and dignity of the elderly.
Physical and emotional signs of abuse are often the most apparent. Unexplained injuries, such as bruises or fractures, and sudden changes in behavior or mood can indicate physical or emotional abuse. Recognizing these signs is key to early intervention and prevention of further harm.
Indicators of financial exploitation are less obvious but equally harmful, such as:
- Unusual withdrawals from bank accounts
- Sudden changes in financial documents
- Unexplained expensive gifts to others
Reporting abusive behavior is a critical step in protecting elderly patients and preventing further mistreatment. The first step in reporting elder abuse is to contact local authorities, such as:
- San Bernardino County Sheriff's Department
- California Adult Protective Services
- California Department of Social Services
- California Department of Public Health
These agencies are equipped to investigate abuse allegations and take necessary protective actions. Providing detailed information and any available evidence is crucial for an effective response.
In addition to reporting to authorities, legal recourse is available for victims and their families. Consulting with a San Bernardino County nursing home attorney can guide legal options, including filing a lawsuit for damages. Legal action creates a pathway to seek compensation for the victim and serves as a deterrent against future abuse.
Choosing a Safe Bernardino County Nursing HomeChoosing the right caregiving facility for a loved one is a crucial decision that can significantly impact their quality of life and safety. Understanding the differences between nursing homes and assisted living communities and evaluating the quality of care provided are key factors in making an informed choice.
The distinction between nursing homes and assisted living facilities lies in the medical care and assistance level. While caregiving homes offer more comprehensive care, assisted living facilities typically provide a more independent living environment with some support services.
Evaluating the quality of a nursing home involves examining factors such as:
- Staff-to-resident ratios
- Cleanliness
- Quality of meals
- The overall atmosphere of the facility
Additionally, checking for a history of abuse or neglect and the facility's compliance with state regulations is essential.
The Role of Nursing Abuse AttorneysElder care abuse attorneys play a vital role in advocating for victims and their families. These legal professionals are dedicated to ensuring that victims of abuse receive the justice and compensation they deserve.
Advocating for victims involves more than just legal representation; it includes providing emotional support and guidance through the legal process. Our neglect lawyers are committed to understanding each client's unique situation and tailoring their approach to meet their needs.
Building a strong legal case against nursing home negligence and abuse requires a thorough investigation and evidence gathering. Our San Bernardino neglect lawyers are skilled in uncovering the truth, piecing together the circumstances of the abuse, and presenting a compelling case in court.
Why Choose Our San Bernardino Nursing Facility Abuse LawyersHiring our San Bernardino caregiving home abuse lawyers means selecting a team with a proven track record of success and a deep commitment to justice and fair compensation.
Our experience in handling San Bernardino County nursing facility abuse cases is extensive. We have successfully represented numerous clients, securing the justice they deserve. Our success record speaks to our expertise and dedication to these cases.
Our commitment to justice extends beyond the courtroom. We are dedicated to raising awareness about nursing home negligence and abuse, advocating for policy changes, and ensuring that nursing facilities provide the highest standard of care. We stand firmly on the side of the victims and their families, fighting tirelessly to protect their rights and interests.
Contact Our San Bernardino County Nursing Home Abuse AttorneysContacting our San Bernardino County nursing home abuse attorneys is a crucial step in seeking justice for abused victims.
Scheduling a free consultation with our personal injury law firm is easy. During this consultation, we will review your case, answer your questions, and discuss how we can help you and your loved one.
Our promise to our clients is unwavering: we will fight tirelessly to protect your rights and seek the monetary recovery you deserve. We understand the emotional and physical toll that nursing home negligence and abuse can take, and we are here to support you every step of the way.
Contact our nursing home abuse lawyers at (800) 926-7565 to schedule a free consultation with an experienced San Bernardino County nursing facility abuse attorney.
 San Bernardino County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
San Bernardino County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
