Search
Nursing Homes With Higher Percentage Of Hispanic Residents Have Higher Rate Of Bed Sores
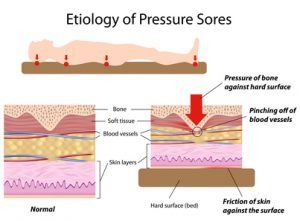
A research study concluded by researchers at Brown University concluded nursing homes with a higher Hispanic populations have higher rates of bed sores (also known as: pressure sores, pressure ulcers, decubitus ulcers) than facilities with less minorities. The results are detailed in the Journal of the American Medical Association.
 The researchers gathered information from the National Repository of the Minimum Data Set, a federally mandated assessment of all nursing home residents and from the Oscar Database System, a survey of all nursing home residents from the Centers for Medicaid and Medicare Services. Additionally, the Brown study evaluated all nursing home residents over 65 who live in nursing homes in California, New Mexico, Texas, Arizona and Colorado.
The researchers gathered information from the National Repository of the Minimum Data Set, a federally mandated assessment of all nursing home residents and from the Oscar Database System, a survey of all nursing home residents from the Centers for Medicaid and Medicare Services. Additionally, the Brown study evaluated all nursing home residents over 65 who live in nursing homes in California, New Mexico, Texas, Arizona and Colorado.
The lead researcher of the Brown survey, Vincent Mor, chair of the Department of Community Health, conducted a similar survey in 2007 that concluded African Americans are more likely than whites to live in poor-quality nursing homes. That study found the disparity of care received in predominately African American nursing homes to be worst in the Midwest.
 Nursing Home Law News
Nursing Home Law News