Search
Even Stiff Fines Can’t Force Nursing Homes To Take Necessary Steps To Prevent Pressure Ulcers
 When nursing homes take simple, preventative steps such as: turning patients, keeping them clean, and providing adequate nutrition and hydration; they can greatly decrease the incidence of pressure sores at their facilities. However, even though the preventative steps are well known, many nursing facilities simply fail to implement the necessary care that patients require to function optimally.
When nursing homes take simple, preventative steps such as: turning patients, keeping them clean, and providing adequate nutrition and hydration; they can greatly decrease the incidence of pressure sores at their facilities. However, even though the preventative steps are well known, many nursing facilities simply fail to implement the necessary care that patients require to function optimally.
I was particularly disturbed when I came across an article in the Arizona Daily Star regarding a Kindred-owned nursing home that has been repeatedly failed to provide sufficient wound care for its patients. In fact, Villa Campana Health Care Center was most recently fined by state authorities $10,000 following a horrific chain of events involving a patient who was admitted to the facility last fall.
Within a month of entering Villa Campana, a patient developed a pressure sore on their buttocks. Despite the staff’s documentation of the wound, little care was provided at the wound progressed to the point that bone was involved and an infection known as osteomyelitis ensued. Eventually, the patient required multiple surgeries to treat the advanced pressure sore including a debridement surgery to remove portions of the coccyx, sacrum and surrounding tissue.
 Nursing Home Law News
Nursing Home Law News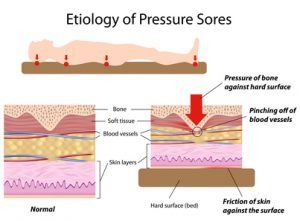






 In times of need, locating necessary information regarding the legal rights and resources for nursing home patients can be difficult and imposing. In this respect, we are proud to introduce a new resource for patients, families and practitioners looking for a concise compilation of information regarding nursing home laws. Nursing Home Injury Laws, provides every states’:
In times of need, locating necessary information regarding the legal rights and resources for nursing home patients can be difficult and imposing. In this respect, we are proud to introduce a new resource for patients, families and practitioners looking for a concise compilation of information regarding nursing home laws. Nursing Home Injury Laws, provides every states’:

