legal resources necessary to hold negligent facilities accountable.
Springfield Nursing Home Abuse Lawyer
 Nursing home abuse is a heinous violation of trust and care, leading to detrimental effects on the health and well-being of elderly patients. This abuse, whether physical, emotional, or psychological, can leave lasting scars and, in severe cases, cause death.
Nursing home abuse is a heinous violation of trust and care, leading to detrimental effects on the health and well-being of elderly patients. This abuse, whether physical, emotional, or psychological, can leave lasting scars and, in severe cases, cause death.
The nursing home abuse attorneys at Nursing Home Law Center, LLC, with their expertise in nursing home abuse cases, are dedicated to protecting the rights of these vulnerable individuals. We work diligently to ensure victims receive their compensation and legal recourse.
Advocating for Elderly Rights and SafetyOur Springfield law firm is deeply committed to advocating for the rights and safety of elderly patients in nursing homes. Our mission as nursing home abuse lawyers is not only to represent victims of abuse and neglect but also to raise awareness about these pervasive issues.
We understand the profound impact that abuse and neglect can have on the residents and are dedicated to providing comprehensive legal support to victims and their families.
Our team of experienced attorneys specializes in handling cases of nursing home abuse and neglect, offering a compassionate and professional approach. We prioritize the well-being of our clients, ensuring that each case is handled with the utmost care and attention to detail. We aim to ensure justice for victims and improve the standard of care in nursing homes across Springfield.
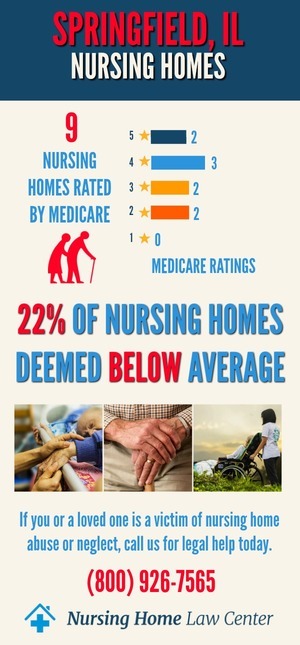
Nursing Home Statistics in Springfield, Illinois: CMS RatingsThe Centers for Medicare and Medicaid Services (CMS) January 2024 updated findings revealed a concerning situation where six out of the 12 facilities assessed, representing 50% of the total, received ratings categorized as "below average" or "much below average" by CMS.
Nursing Home Facilities Cited for AbuseAmong these nursing homes with below-average ratings, some were subjected to additional scrutiny by inspectors who identified instances of abuse and neglect. The following Springfield, Illinois, nursing homes were cited for abuse:
- Arcadia Care Auburn
- Sunny Acres Nursing Home
The presence of below-average-rated nursing homes and instances of abuse underscores the urgency of addressing these issues to protect the vulnerable residents in these facilities.
If you have concerns about a specific facility or require assistance regarding nursing home neglect or abuse, please know our personal injury attorneys are available to advocate for victims harmed through neglect or abuse legally.
The Critical Consequences of Mistreatment in Elder Care FacilitiesIn Rockford, Illinois, the scourge of nursing facility abuse and neglect stands as a stark violation of the inherent dignity and rights of the elderly, leading to severe harm and, in the worst cases, fatalities. Such maltreatment in elder care environments is not just a breach of ethical care but a significant public health concern.
It's critical to acknowledge and understand the following common types of mistreatment, such as the following:
- Physical Abuse: This type of abuse involves the intentional exertion of force that results in physical discomfort, pain, or injury, including actions such as striking, shoving, or restraining beyond medical necessity.
- Sexual Abuse: This refers to any form of non-consensual sexual contact, behavior, or exposure. It is particularly egregious given the vulnerability of the elderly, who may be unable to give consent or protect themselves.
- Emotional and Psychological Abuse: This category covers any conduct that causes mental pain, anguish, or trauma, such as verbal assaults, threats, intimidation, or other forms of emotional manipulation and degradation.
- Neglect: Nursing home neglect is characterized by a caregiver's failure to meet the vital living and healthcare needs of elderly patients, often leading to health deterioration or exacerbation of existing conditions.
- Financial Abuse: This type of abuse involves the misuse or unauthorized taking of a resident's monetary resources or property, often characterized by sudden changes in financial documents or unexplained disappearance of funds or valuables.
- Medical Malpractice: This occurs when substandard medical care is provided, including errors in medication administration, insufficient health care provision, or neglect in routine medical procedures, which can result in serious health outcomes.
- Abandonment and Isolation: Forcing patients into solitude or ignoring their need for social interaction and care constitutes abandonment and isolation. Such practices can lead to emotional distress and rapid health decline due to a lack of social and medical stimuli.
In recognizing these distressing forms of abuse, it is crucial for family members, caregivers, and the broader community to remain vigilant and to act decisively to protect the health and rights of nursing home residents.
Mistreatment Signs and SymptomsIdentifying the warning signs of nursing home mistreatment to ensure resident safety is crucial. Vigilance in observing symptoms is the first line of defense against further harm.
Physical Indicators:- Unexplained injuries such as bruises, cuts, or fractures.
- Sudden weight loss or gain may indicate nutritional neglect.
- Poor hygiene, indicating a lack of assistance with daily living activities.
- Withdrawal from social interactions, possibly signaling psychological abuse.
- Sudden changes in mood or behaviors, which may be responses to abuse.
- Uncharacteristic aggression or agitation, potentially stemming from elder abuse.
- Noticeable decline in cleanliness within the living facility, hinting at neglect cases.
- Lack of necessary medical aids like glasses or dentures, pointing to inadequate care.
- Bed sores, pressure sores, or other untreated medical conditions suggest nursing home neglect.
- Unexplained withdrawals or changes in financial documents signify financial abuse.
Addressing these issues promptly can prevent further abuse, save on potential medical bills, and ensure that many facilities provide the adequate care and respect that elderly loved ones rightfully deserve.
Addressing the Multifaceted Impact of AbuseIn Springfield, Illinois, and throughout Central Illinois, recognizing and understanding the symptoms and consequences of nursing facility abuse is imperative.
Physical and Health Ramifications:- Immediate medical concerns such as injuries sustained from resident falls or resident falling incidents.
- Long-term health issues, including unexplained weight loss or complications from neglect.
- Enduring psychological trauma, which can manifest as depression or anxiety.
- Loss of trust in nursing home caregivers or other residents affects social relationships.
- Incurred medical expenses due to treatment for injuries or wrongful death.
- There is a potential need for legal intervention, calling for a nursing home abuse lawyer to pursue justice on a loved one's behalf.
- Law firms specializing in elder care issues offer free consultations to discuss legal options.
- A Springfield, IL, nursing home abuse attorney can help navigate Illinois law, advocating for adequate care and compensation.
- Legal teams can assist with recovering costs, from ongoing medical treatment to funeral costs, and seek accountability from negligent facilities.
Family members must be equipped to take decisive action, including reporting to the Illinois Department of Public Health or consulting with personal injury lawyers to explore all legal options. It is through a combined effort that we can protect our elderly loved ones from harm and ensure that those responsible for nursing home neglect or abuse are held accountable.
The Critical Role of Reporting Elder Care Facility MisconductIn the realm of elder care, the responsibility to report misconduct within nursing homes and assisted living facilities is a vital one. Reporting acts of nursing home neglect or abuse can be lifesaving, reinforcing the respect and safety owed to our elderly loved ones.
When misconduct is reported promptly, it triggers formal inquiries that hold facilities accountable and create a safer, more dignified environment for all nursing home patients.
If you find yourself confronting signs of abuse or suspect neglect cases in any nursing home environment, Central Illinois offers several dedicated channels for reporting. Springfield, IL, patients and those in the surrounding areas have access to both national and state resources equipped to address and investigate these serious concerns:
- Illinois Department of Public Health's Nursing Complaint Hotline: Patients and their families can report concerns by dialing 1-800-252-4343. The number for issues within Supportive Living Facilities (SLF) is 1-800-226-0768.
- Medicaid Fraud, Abuse, or Neglect Hotline: To address incidents involving Medicaid services, contact 1-888-557-9503.
- Department of Human Services' Office of the Inspector General (OIG) Hotline: For abuse or neglect of individuals with mental illness or developmental disabilities in DHS-operated facilities, the hotline is 1-800-368-1463.
- Senior HelpLine: This line is open for reporting suspected abuse or neglect at (800) 252-8966 or (888) 206-1327 for TTY users.
- Illinois Department of Public Health (IDPH): Complaints concerning nursing home negligence or abuse can also be filed directly with the IDPH at 800-252-4343 or 800-547-0466.
Each of these agencies plays a pivotal role in safeguarding the rights and well-being of elderly residents. They are essential to overseeing nursing home facilities, ensuring a proper standard of care is administered and that violations are dealt with swiftly and justly.
When seeking assistance, you may consult a Springfield nursing home abuse lawyer who can provide a free consultation and help navigate the legal landscape, offering representation and support through potential negligence cases.
Legal Expertise and RepresentationOur law firm provides specialized legal expertise and representation in nursing home negligence and abusive behavior cases. We are committed to offering the best legal solutions to our clients, ensuring their rights are protected.
Navigating Legal Recourse for Nursing Home Abuse and NeglectSeeking the expertise of attorneys who specialize in elder care home abuse and negligence is a critical step in safeguarding your loved ones from further mistreatment.
Such legal professionals are advocates and protectors armed with the knowledge and skills to navigate the often-complex waters of elder abuse law. Their role is instrumental in halting the cycle of abuse and ensuring that the rights and dignity of the most vulnerable are upheld.
Comprehensive Case EvaluationEngaging with lawyers who specialize in elder abuse begins with an in-depth evaluation of the incident. This critical step involves a detailed examination of medical records, an analysis of witness testimonies, and an extensive review of all evidence to construct a robust legal strategy.
Guidance Through the Litigation JourneyThe path to justice in cases of nursing home mistreatment can be daunting. Experienced attorneys serve as navigators, guiding clients through each phase of the legal process. From the initial filing of a lawsuit to the intricacies of courtroom dynamics, these legal professionals are steadfast in their mission to secure the best possible outcomes for those they represent.
Achieving Maximum CompensationIn discussing the potential avenues for resolution, attorneys will explore the possibilities of both settlements and verdicts. The aim is to conclude that it not only offers fair restitution for the harm suffered but also serves as a deterrent against future occurrences of abuse.
The goal is twofold: to procure justice for the individual victim and their family and to contribute to the broader imperative of improving standards across nursing homes.
In essence, partnering with a specialized legal team can provide a beacon of hope and a means of recourse for families grappling with the aftermath of nursing home abuse. These legal experts stand as vigilant defenders, ready to assert the rights of your loved ones and to fight for the respect and care they are rightfully owed.
Our Commitment to Justice and ChangeOur law firm is committed to winning cases and advocating for systemic changes in nursing home care standards. We aim to make a lasting impact in the lives of our clients and the community.
We stand as staunch advocates for the rights and dignity of victims of elder care home abuse. Our attorneys work tirelessly to ensure that our clients' voices are heard and that they receive the justice they deserve.
Our efforts extend beyond individual cases. We are dedicated to bringing about positive changes in nursing home care standards, ensuring that elderly patients receive the respect and care they are entitled to.
Springfield Nursing Home Abuse Frequently Asked QuestionsWhen the safety and well-being of a nursing home resident are compromised due to negligent or intentional acts, it's crucial to seek the expertise of a Springfield nursing home negligence attorney.
Our Springfield, IL, law firm is committed to protecting the rights of the elderly in nursing homes and assisted living facilities, ensuring they receive the proper care and respect they deserve.
If your loved one has suffered from nursing home neglect or abuse, you are not alone. At Nursing Home Law Center, LLC, we understand the pain and urgency of addressing such grave concerns. Our dedicated nursing home abuse lawyers are committed to protecting the rights and dignity of nursing home residents throughout Central Illinois, including Springfield.
With a focus on providing top-tier legal representation, we fight to secure the proper care and justice your family member deserves. From issues in assisted living facilities to the warning signs of a neglect case, our staff members are equipped with relevant information to guide you through the process.
Contact our nursing home abuse lawyers now at (800) 926-7565 for a free consultation. We operate on a contingency fee basis, which means you save money as we only get paid if you win. Let a competent Springfield, IL, nursing home abuse attorney advocate for your loved one and ensure that the nursing homes fail to overlook their duty of care no longer.
 Sangamon County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Sangamon County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
