legal resources necessary to hold negligent facilities accountable.
Utah Nursing Home Abuse Lawyer
Nursing home abuse or neglect takes many forms, and it is important for family members to have a comprehensive overview of this societal issue before enrolling loved ones in a facility.
Knowing how abuse occurs, the legal rights of loved ones and how to report abuse can empower family members to take action if it is ever necessary in an abusive situation.
First off, nursing home abuse can occur in the physical, mental, verbal or sexual forms. Nursing home neglect also can impact residents, and it refers to a lack of adequate care that causes harm in the lives of nursing home patients.
Residents can develop bedsores or ulcers due to a lack of movement, improper transitions or improperly trained staff.
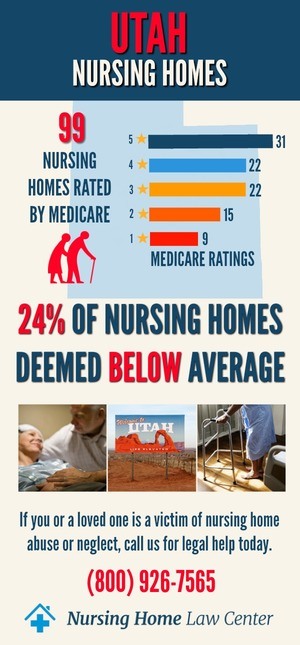
Throughout the year, Medicare routinely gathers data on the 102 nursing homes rated in Utah through surveys, inspections and investigations into formally filed complaints. The federal agency states that currently, twenty-two (22%) of these nursing homes are deemed to provide substandard care based on identified violations and deficiencies.
Abuse or Neglect at a Care Facility
Was your loved one injured, mistreated, abused or did they die unexpectedly from neglect while residing in a Utah nursing home?
If so, we invite you to contact a Utah nursing home abuse attorney at Nursing Home Law Center today to discuss a case for compensation. We offer every potential client a free case review.
In Utah, over one-third of all nursing homes have deficiencies in the professional standards, food sanitation and in maintaining a safe environment for nursing home residents. In 2008, researchers from the University of California-San Francisco found that over 21 percent of all nursing homes provided unnecessary drugs to our elders. Unnecessary drugs can be referred to as “chemical restraints,” and they are used as a way to control the behavior of residents in difficult situations.
It is illegal to administer drugs to nursing home residents as a way for staff members to sedate their behavior or try to control their movements.
If you discover that your loved one has been forced to consume chemical restraints, then you should get in touch with Salt Lake City nursing home abuse lawyers today. Utah nursing home abuse lawyers are available to investigate your loved one’s case and protect him or her.
Nursing Home Abuse and Injury Laws in Utah
In Utah, there are nursing home abuse and personal injury laws in place to protect the rights of residents.
Family members have a total of four years to file a nursing home negligence case within the time of first discovering a personal injury on a loved one. For a medical malpractice case, the time period is for two to four years.
Family members may only obtain non-economic damages in medical malpractice actions for up to $400,000.
For a wrongful death case, family members only have a limited time of two years in which to file a claim. This means that if your relative has died from abuse or neglect, then you should speak to nursing home injury lawyers as soon as possible to file your claim. One can only receive up to $400,000 for non-economic damages in medical malpractice claims.
The two statutes that are in place to protect the legal rights of residents are the Adult Protective Services Act and the Abuse, Neglect or Exploitation of a Vulnerable Adult Act.
For individuals who have engaged in the abuse of a vulnerable adult, there may be a felony charge if the abuse has been intentional. If a vulnerable adult was exploited in a negligent or reckless manner, then a worker may be guilty of a misdemeanor charge.
Call Our Personal Injury Law Firm to Fight for the Legal Rights of Your Loved Ones
It is essential to fight for the legal rights of your loved one when you have discovered that he or she has been victimized in an abusive situation.
No family member should have to suffer from physical abuse or exploitation due to the elder rights law in Utah.
If your loved one has suffered from injuries in an abusive situation, then he or she may be entitled to receive a large sum of compensation.
A loved one may be able to receive compensation for the following types of injuries:
- Broken or fractured limbs
- Abrasions and open wounds
- Severe scratches or burns
- Major concussions
- Wrongful death arising from a personal injury
Free Consultations from a Utah Nursing Home Injury Lawyer Today
You can call one of our Utah nursing home abuse and personal injury lawyers to receive immediate assistance for your case and learn about elder rights law in Utah.
Know the types of legal claims that may be available to you and your relative with the help of a nursing home lawyer.
Our attorneys are available to help families throughout Utah with nursing home abuse cases in areas such as:
- Layton
- Ogden
- Orem
- Provo
- Salt Lake City, UT
- Sandy
- St. George
- West Jordan
- West Valley City
You may be eligible to file a negligence claim, or a nursing home lawyer may be able to settle your claim outside of court.

Utah Nursing Home Lawyers Serving Victims of Bed Sores, Pressure Sores & Decubitus Ulcers
Many Utah nursing home patients are victims of serious pressure sores where their lives are placed at risk by the medical staff’s negligence.
Fortunately, with the best medical care, most pressure sores can be prevented easily when the medical team follows three basic steps, which include:
- Perform regular daily skin inspections
- Keep the resident dry and clean at all times
- Ensure that the resident is receiving quality nutrition and is fully hydrated to boost their immune system
Nearly every type of issue involved with a developing pressure sore (bedsore; pressure ulcer; decubitus ulcer) can be prevented when the medical team at a nursing home performs a routine inspection on the patient’s skin.
By inspecting body parts, especially bony prominences, any potential developing bedsore can be easily recognized while in the early stage.
Legal Advice for Bedsores
The most common places for a bedsore to develop on the body include bony areas such as the shoulders and shoulder blades, head, heels, ankles, buttocks, sacrum, hip bones and spine.
The medical community categorizes pressure sores into specific stages from minimal to life threatening. These stages include:
- Stage I –In its initial stage, a pressure sore will appear on the body as a reddened area with or without blisters and red dots. The complete healing process can begin by alleviating the pressure, and keeping it off the area until the wound is resolved.
- Stage II –When the medical team allows an early-stage bedsore to advance to the next level, a shallow crater appears on the skin surface at the affected area. Fatty deposits may also be present. Effective treatment requires specialized wound dressings to decrease the potential of infection.
- Stage III -At this stage, the pressure sore begins to ulcerate significantly, causing a deep crater at the site. Infection is likely unless intervention is taken, including the use of prescribed antibiotics.
- Stage IV –If the antibiotics are ineffective or not prescribed, the bedsore can easily advance to a crucial life-threatening decubitus ulcer where the patient’s health is greatly compromised. Healing at this stage, if possible, usually requires outside medical intervention by teams of specialists competently trained in treating life-threatening bedsores.
In many incidences, patients with advanced stage pressure ulcers die from sepsis (blood infection) or osteomyelitis (bone infection).
Call (800) 926-7565 Toll-Free for a No Obligation Consultation

An Indication of Neglect and Inferior Care at Medical Facilities
Medical science has long established the proven protocols necessary to minimize the potential of an initial bedsore progressing to an advanced stage.
Because of that, nearly every Stage II to Stage IV is an indicator of neglect at the nursing facility.
Had the staff followed protocol by routinely monitoring the patient’s skin every day, ensuring that their body is readjusted every two hours or less, the advancement of the bedsore could likely have been prevented.
Because of that, many families will hire a Utah pressure sore lawyer to stop the negligence immediately.
An attorney can handle the claim for financial compensation and begin the process of building a case to hold all responsible parties accountable for their negligence.
This includes obtaining medical charts to look for any detailed notes of a bedsore and any actions taken or not taken by the medical staff to treat the condition.
In addition, the law firm can send in a team of medical personnel with specialized knowledge of treating severe decubitus ulcers.
These professionals provide these life-saving services in cities all throughout Utah including:
- Salt Lake City
- West Valley City
- Provo
- Sandy
- Orem
Frequently Asked Questions About Nursing Home Personal Injury Lawsuits
Here are the answers to some commonly asked questions that families have about nursing home abuse lawsuits:
How Much Is My Nursing Home Lawsuit Worth?
This all depends on how much your individual family member has suffered. A settlement or jury award would include:
- Pain and suffering
- Emotional trauma
- Wrongful death
- Possible punitive damages
A consultation with experienced nursing home abuse attorneys can assist in determining the value of the case.
How Long Does My Nursing Home Abuse Lawyer Have to File a Lawsuit?
In Utah, the personal injury statute of limitations for nursing home abuse or neglect cases is four years. If the case involves medical malpractice or wrongful death, the time limitation may be as short as two years. If you miss the deadline, you lose the ability to file a lawsuit.
How Much Does it Cost to Hire Our Law Firm?
Absolutely nothing upfront. You do not need to write us a check for a retainer or pay us by the hour. We are only paid if you are successful in your nursing home abuse lawsuit. If you do not recover, we are not paid.

Attorneys for Nursing Home Negligence in Salt Lake City and Utah
If you and your family suspect that the nursing staff was negligent and caused your family member to suffer a bedsore, it is essential to speak with a Utah pressure sore lawyer. Fill out the form here to schedule an appointment with one of the reputable law firms listed below. To avoid the need for any upfront fees, your attorney will take your case on contingency. The law firm can file a claim or lawsuit demanding financial recompense for the injuries and damages your family member has endured. We can give you legal advice as soon as the attorney client relationship begins.
Call Us for a Free Consultation
Call our phone number at (800) 726-9565 to reach an abuse lawyer with years of experience helping people across the state.
Nursing Home Negligence
STATUTE OF LIMITATIONS
- 4 years with Discovery Rule. (Utah Code Ann. §78B-2-307)
- Medical malpractice – 2 years with Discovery Rule, but no more than 4 years from the date of the alleged act, omission, neglect, or occurrence. In foreign object cases, suit must be filed within one year from the date the plaintiff discovered or should have discovered the object. These limitations also apply to minors under eighteen. (Utah Code Ann. §78B-3-404)
DAMAGES CAP
- Noneconomic damages in medical malpractice arising after July 1, 2002 are limited to $400,000, adjusted annually for inflation. (Utah Code Ann. §78B-3-410)
WRONGFUL DEATH STATUTE OF LIMITATIONS
- 2 years with Discovery Rule. (Utah Code Ann. §78B-2-304 – Within two years)
DAMAGES CAP
- Noneconomic damages in medical malpractice arising after July 1, 2002 are limited to $400,000, adjusted annually for inflation. (Utah Code Ann. §78B-3-410 )
State Resources
- Utah Department of Health
- Bureau of Health Facility Licensing, Certification, and Resident Assessment
Nursing Home Care State Law
- Abuse, Neglect, or Exploitation of a Vulnerable Adult – Penalties (Utah Code Ann. §76-5-111.1)
 Utah Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Utah Nursing Home Injury Attorney Nursing Home Law Center LLC Home



