legal resources necessary to hold negligent facilities accountable.
Detroit Nursing Home Abuse Lawyer
The prevalence of abuse and neglect in nursing homes poses a significant threat to the health and dignity of elderly residents. Such misconduct not only compromises their physical health but also inflicts psychological trauma, diminishing their quality of life.
At the Nursing Home Law Center, LLC, we provide a platform for the victims and their families to understand their rights and options. Our team of nursing home abuse lawyers works tirelessly to advocate for the rights of the elderly, ensuring that abusive and negligent practices are brought to light and addressed.
Upholding the Rights of the Elderly in Nursing HomesThe proliferation of misconduct by nursing home staff and the subsequent need to hold the nursing home accountable underline the critical work of a nursing home abuse attorney. In Detroit, where such incidents have seen an alarming rise, the elderly population is particularly vulnerable.
Nursing Home Law Center, LLC is at the forefront of addressing these issues, ensuring that every elderly person's dignity and rights are vehemently protected within these institutions. Our specialized attorneys and legal professionals are dedicated to providing unwavering support and expertise to the victims and their families.
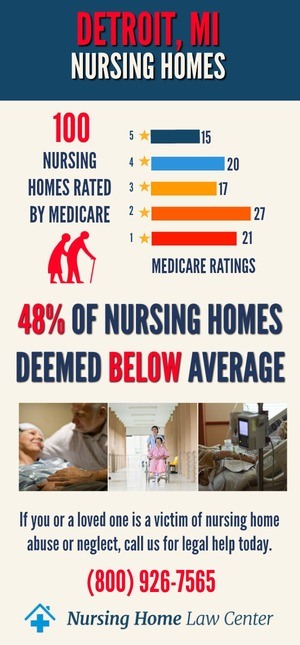
Detroit, Michigan Nursing Home Statistics from CMSIn February 2024, the Centers for Medicare and Medicaid Services (CMS) updated its comprehensive evaluations of nursing homes in Detroit, Michigan. The findings revealed a profoundly concerning situation, as 56 out of the 116 facilities in the city, which accounts for a staggering 48%, were rated as either "below average" or "much below average" according to CMS standards.
This concerning statistic underscores the critical importance of government agencies in monitoring and addressing issues related to nursing home neglect and abuse.
Nursing Homes Cited for AbuseWithin this distressing statistic, it's important to highlight specific nursing homes that inspectors have cited for abuse. The following facilities have come under scrutiny for various reasons, and it is crucial to bring attention to their names:
- Beaconshire Nursing Centre
- Lakeland Center Nursing Center
- Marvin & Betty Danto Health Care Center
- Medilodge of Southfield Nursing Care Center
- Medilodge of Sterling Heights Nursing Care Center
- Mission Point Nursing and Physical Rehabilitation Center of Beverly Hills
- Mission Point Nursing and Physical Rehabilitation Center of Clawson
- Mission Point Nursing and Physical Rehabilitation Center of Elmwood
- Mission Point Nursing and Physical Rehabilitation Center of Madison Heights
- Mission Point Nursing and Physical Rehabilitation Center of Warren
- Notting Hill of West Bloomfield Nursing Care Center
- Optalis Health and Rehabilitation of Troy
- Regency at Canton Nursing Facility
- Regency at Shelby Township Nursing and Medical Care Center
- St. James Nursing Center
- The Orchards at Roseville
- The Villa at City Center
Government agencies, including CMS, are vital to nationwide surveying and inspecting nursing facilities. The primary reason for this oversight is to ensure the safety and well-being of nursing home residents.
Nursing home neglect and abuse can manifest in various forms, such as physical abuse, emotional abuse, medical neglect, and the administration of the wrong medication. These distressing acts can result in severe harm to elderly persons living in nursing facilities, making it imperative that these institutions provide the highest practicable physical and mental well-being for their residents.
Agencies you can report suspected abuse or neglect include:
- Michigan Department of Attorney General Elder Abuse, Neglect, and Exploitation Call 1-800-24-ABUSE (22873)
- Michigan Department of Health and Human Services and Adult Protective Services
- National Center on ElderAbuse 1-855-500-3537 (ELDR)
In addition to routine inspections, government agencies respond to formal complaints filed by nursing home residents and their families. These complaints may pertain to a wide range of issues, including nursing home abuse cases and instances of negligence. Government agencies conduct thorough investigations to ensure that nursing facilities are held accountable for any wrongdoing.
Legal Action and Nursing Home Abuse AttorneysWhen nursing home residents or their families believe that their loved ones have suffered injuries or harm due to negligence or abuse, they have the right to seek legal action. Skilled nursing home abuse attorneys specialize in handling cases of this nature and play a pivotal role in advocating for the rights of the victims and their families.
Seeking Justice and CompensationLegal action against nursing care homes that have been negligent or abusive can result in financial compensation for the victims and their families. This compensation may cover medical expenses, pain and suffering, and other damages incurred due to the abuse or neglect. Working alongside insurance companies, personal injury lawyers assess the evidence, determine liability, and strive to ensure justice.
Empowering Families with Knowledge and Legal SupportThe statistics from CMS's evaluation of nursing care homes in Detroit, Michigan, raise a significant concern about the quality of care provided to our elderly population. Government agencies serve as a vital safeguard against nursing home neglect and abuse.
Patients' families must be aware of their legal rights and the resources available to them, including skilled nursing abuse attorneys seeking justice and compensation for victims of nursing home abuse and neglect.
By taking action and holding nursing homes accountable, we can work toward ensuring that our elderly loved ones receive the care and respect they deserve in assisted living facilities throughout Detroit, Wayne County, and the state of Michigan.
Nursing Home Abuse and Neglect: Protecting Our EldersThe issue of nursing home neglect and abuse in the Detroit area is not only alarming but also indicative of a significant systemic failure to protect our most vulnerable population. Our nursing abuse attorneys see the devastating impact such neglect can have on disabled and elderly residents and their family members.
Our firm's mission is rooted in the commitment to advocate for the rights of these individuals, ensuring that they receive the adequate and appropriate care they deserve.
Ensuring the Safety and Dignity of Elderly ResidentsEvery elderly resident living in a nursing care facility or assisted living facility is entitled to a safe, nurturing environment. However, the reality often falls short of these expectations. Instances of physical assault, emotional abuse, and medical malpractice are all too common, leaving the victims and their families in dire need of professional legal assistance.
Our nursing home abuse lawyers are well-versed in the intricacies of Michigan nursing home regulations and are dedicated to holding negligent facilities accountable.
Empowerment Through Awareness and Legal SupportThe first step in combating nursing home abuse is recognizing the signs and understanding the rights of the elderly. Our law firm provides a free consultation to family members and victims, offering a compassionate ear and expert advice on the best course of legal action.
We believe that raising awareness and providing solid legal representation can significantly improve the standards of care in Michigan nursing homes.
Definition and Types of AbuseAt the heart of our legal practice is a deep understanding of the various forms of abuse that can occur within nursing care homes. Our Detroit nursing home abuse lawyer team categorizes abuse into several types, including the following:
- Physical Abuse: This involves any intentional act causing injury or harm to a nursing home resident, such as hitting, pushing, or improper restraint use. The physical signs, including unexplained bruises or broken bones, can often be the first indicators of such abuse.
- Sexual Abuse: Unwanted or non-consensual sexual contact with a nursing home patient, which is a gross violation of their rights and dignity. This type of abuse can leave deep psychological scars alongside any physical harm.
- Emotional Abuse: Often more difficult to detect, this form of abuse includes verbal assaults, threats, or other actions that inflict emotional pain or distress on the elderly, undermining their psycho-social well-being.
- Financial Abuse: Illegal or unauthorized use of an elderly person's finances or property, including stealing cash, forging signatures, or misusing the resident's financial accounts.
- Negligence: Failing to provide primary care needs, leading to issues like pressure sores, malnutrition, or hygiene problems. Nursing home negligence can stem from inadequate staffing or poor training of staff members.
- Medical Malpractice: This encompasses errors in medical treatment, from incorrect medication administration to failure in diagnosing or treating health conditions, resulting in harm or even death.
Our law firm leverages its professional experience in nursing home abuse cases to navigate these complex issues, ensuring that the victims and their families receive their deserved justice and compensation.
Prevalence of Nursing Home Issues in DetroitDetroit's unique socio-economic landscape contributes to specific challenges in the realm of nursing care. Our Detroit nursing abuse attorneys have observed a worrying trend in the prevalence of abuse and neglect cases within the city, pointing to systemic issues that require comprehensive legal and policy responses.
Early identification of abuse signs is crucial for intervening and stopping further harm to facility residents. Our personal injury law firm educates clients on the various indicators of abuse, from sudden changes in behavior to unexplained injuries, and how to document these signs for legal action.
Detroit's Senior Population and Its Unique NeedsThe demographics of Detroit's senior population highlight unique vulnerabilities that can increase the risk of abuse. Our nursing home abuse attorney team considers factors such as socio-economic status, health conditions, and familial support systems when building personal injury cases to ensure that all aspects of a resident's needs are considered.
Impact of Profit-Driven Care on Elderly PatientsThe rise of profit-driven motives in some nursing facilities often comes at the expense of quality care and safety for residents. Our Detroit nursing home abuse law firm critically analyzes the policies and practices of these facilities to uncover instances where the pursuit of profit leads to neglect and abuse.
Legal Recourse for Nursing Home Abuse VictimsEvery victim of nursing home abuse in Detroit has various legal avenues to seek justice and compensation. Our attorneys are proficient at guiding clients through the complexities of the legal process, from filing a nursing home abuse lawsuit to representing them in court or settlement negotiations.
Navigating Legal Options, Promoting Awareness and Preventive MeasuresUnderstanding the legal rights of nursing home abuse victims is paramount. Our law firm provides comprehensive counsel on these rights and the best strategies for legal recourse, ensuring that our clients are fully informed and prepared for the legal journey ahead.
Preventing abusive behavior and negligence requires a multifaceted approach, including community education and legal advocacy. Our law firm is active in promoting awareness about the signs of abuse and the legal protections available to the victims and their families, aiming to prevent abuse before it occurs.
Choosing the Right Nursing HomeSelecting the right nursing facility is a critical decision that can significantly impact the well-being of elderly family members. Our attorneys offer guidance on evaluating nursing facilities, from assessing the quality of care to understanding residents' rights to helping families make informed choices.
Ensuring safe and dignified living conditions for seniors involves considering various factors, from the facility's staffing levels to its history of compliance with regulations.
Hire a Nursing Home Abuse Lawyer Advocating for the ElderlyIs your beloved family member the victim of nursing home abuse and neglect? At Nursing Home Law Center, LLC, our unwavering commitment is to advocate for the rights and well-being of the elderly in Detroit nursing homes.
We stand ready to support victims of abuse and their families, offering expert legal representation and a compassionate approach to each case, ensuring that justice is served and dignity is restored.
Contact our nursing home abuse lawyers at (800) 926-7565 to schedule a free consultation. We accept all cases on a contingency fee agreement, meaning you pay no upfront fees until your personal injury lawyer wins your case.
 Wayne County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
Wayne County Nursing Home Injury Attorney Nursing Home Law Center LLC Home
