legal resources necessary to hold negligent facilities accountable.
Knoxville Nursing Home Abuse Lawyer
 The prevalence of nursing home abuse is an alarming reality that demands immediate and decisive action. This abuse, ranging from neglect to outright physical harm, can leave lasting psychological and physical scars on its victims.
The prevalence of nursing home abuse is an alarming reality that demands immediate and decisive action. This abuse, ranging from neglect to outright physical harm, can leave lasting psychological and physical scars on its victims.
At Nursing Home Law Center, LLC, we specialize in uncovering and addressing these injustices. Each Knoxville nursing home abuse lawyer works tirelessly to ensure that victims receive the compensation they deserve and that measures are taken to prevent future abuse.
Knoxville Nursing Home Abuse Lawyers Championing Justice for Vulnerable SeniorsNursing home abuse in Knoxville is a distressing reality that affects some of our community's most vulnerable members. We understand the profound impact that such abuse can have on an elderly person and their loved ones, and we strive to hold responsible parties accountable for their actions.
The prevalence of elder abuse and neglect in Knoxville and the surrounding areas is a matter of grave concern. By holding negligent parties accountable and advocating for improved care standards, we can work toward ensuring the safety and well-being of elderly residents in Knoxville, Tennessee. Our legal team is dedicated to addressing this issue head-on, providing compassionate yet aggressive representation to those affected.
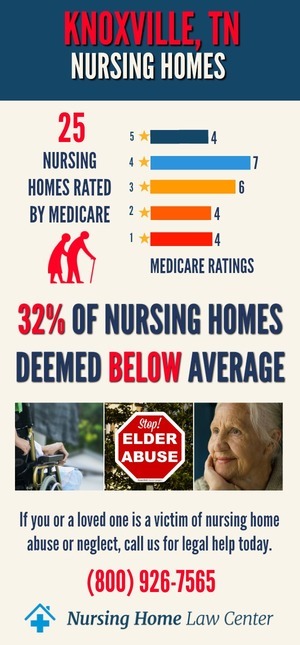
 Troubling Nursing Home Statistics in Knox County, Tennessee
Troubling Nursing Home Statistics in Knox County, TennesseeAs of December 2023, Knoxville, Tennessee, is grappling with a concerning issue in its nursing homes. The Centers for Medicare and Medicaid Services (CMS) statistics reveal that a staggering 54% of the 28 nursing homes in Knoxville are rated as "below average" or "much below average." These statistics show the pressing need for improved care standards and safety measures in the city's long-term care facilities.
Inspectors' Findings and Cited FacilitiesAmong the nursing homes in Knoxville, several have been cited for instances of abuse, further emphasizing the need for action. These facilities include:
- Beverly Park Place Health and Rehab
- Fairpark Health and Rehabilitation
- NHC Healthcare Knoxville
- Shannondale Health Care Center
- Summit View of Rocky Top
- Westmoreland Health and Rehabilitation Center
These inspections' findings underscore the urgent need for enhanced care, nursing home resident safety, and accountability in Knoxville's professional caregivers. Families of nursing home patients must be vigilant. With the assistance of Knoxville nursing home abuse lawyers, they can explore their legal rights and pursue compensation for any injuries or harm experienced by their loved ones in these facilities.
 Protecting Your Loved One's Rights
Protecting Your Loved One's RightsThe protection of your loved one's rights in a Knoxville nursing home is our top priority. We recognize that entrusting a family member to the care of a nursing facility is a significant decision. When that trust is breached through abuse and neglect, it is devastating. Our legal team works tirelessly to ensure that the rights of nursing patients are upheld and respected.
Legal Framework and Patient RightsThe legal framework surrounding nursing facility care provides essential protections for elderly residents. Understanding these laws and regulations is crucial for ensuring that nursing facilities adhere to the required standards of care.
- Federal and State Laws: Safeguarding nursing patients against abuse and neglect.
- Patient Rights: Ensuring residents receive respectful and competent care.
Legal advocacy is crucial in safeguarding the rights of the elderly in nursing homes. Nursing facility abuse lawyers play a pivotal role in navigating the complexities of such cases, ensuring that victims receive proper representation. Our firm understands the importance of legal intervention, especially when facilities fail to provide a safe environment or proper medical care, leading to injuries that residents sustain.
 Understanding Your Options for Reporting Abuse
Understanding Your Options for Reporting AbuseWhen faced with the unfortunate reality of nursing facility abuse, it's crucial to know the appropriate steps to take. The importance of reporting such incidents cannot be overstated, as it not only helps protect the victim but also prevents future cases of abuse. Understanding where and how to report abuse and who to contact is the first step toward ensuring the safety and well-being of our elderly loved ones.
Reporting Channels for Nursing Home Abuse- State's Ombudsman Program: This program assists and advocates for care home residents. The Ombudsman investigates complaints and works toward resolving residents' health, safety, welfare, and rights issues.
- Tennessee Department of Health: The Department oversees nursing home regulations and investigates allegations of abuse, neglect, or mistreatment.
- Law Enforcement: In cases of immediate danger or severe abuse, contacting the local police at 911 is essential. They can provide immediate assistance and ensure the safety of the victim.
- Tennessee Department of Human Services Adult Protective Services: This department investigates reports of elder abuse, neglect, or exploitation of adults unable to protect themselves due to mental or physical limitations.
- Tennessee Commission on Aging and Disability: This commission is an advocacy group dedicated to addressing the needs of older adults and people with disabilities. Reporting abuse to them can ensure that the victim receives the necessary support and that systemic issues within the care home are addressed.
- Nursing Home Law Center, LLC: Our personal injury law firm represents victims of nursing home mistreatment, abuse, and neglect. We provide legal advice and representation to ensure that victims receive the justice and financial redress they deserve through a nursing home abuse claim. Our team of experienced attorneys can guide you through the legal process and help hold the responsible parties accountable.
- Other Relevant Authorities: Depending on the nature and severity of the abuse, it may be appropriate to reach out to additional agencies or legal professionals specializing in elder abuse.
Remember, taking the step to report abuse is a vital action in protecting some of the most vulnerable members of our society. If you suspect nursing home mistreatment, abuse, or neglect, do not hesitate to reach out to these resources.
 Understanding Nursing Home Abuse
Understanding Nursing Home AbuseUnderstanding the various forms of abuse is essential for identifying and addressing these issues effectively. Our Tennessee nursing home abuse lawyers are well-versed in the different types of abuse that can occur within these facilities. We are prepared to provide legal support to victims and their families.
Nursing Home Residents: Different Forms of Abuse- Physical Abuse includes hitting, slapping, or using unnecessary physical restraints.
- Emotional Abuse and Psychological Abuse can manifest as intimidation, social isolation, verbal insults, and other verbal abuse.
- Sexual Abuse involves any non-consensual acts or indecent exposure.
- Financial Abuse: Unauthorized use of a resident's financial resources.
- Healthcare Fraud involves unethical practices like overbilling or unnecessary medication.
- Nursing Home Negligence can involve injuries sustained from a lack of personal hygiene assistance, medication mistakes, or help with activities of daily living (feeding, mobility, etc.) by nursing staff members.
Recognizing the signs of abuse is critical in taking timely action to protect disabled and elderly patients. Being aware of these indicators can help in identifying cases of abuse and neglect early, preventing further harm.
Identifying Mistreatment Involving Unexplained Injuries- Physical Abuse Indicators: Unexplained bruises, broken bones, weight loss (malnutrition), or poor hygiene.
- Emotional and Psychological Signs: Signs of depression, anxiety, or withdrawal.
- Medical Neglect: Any negligence by medical professionals (medical malpractice), including nursing home staff members, can cause severe injury when their actions or lack of actions lead to a severe medical condition.
- Financial Irregularities: Sudden changes in financial status or missing valuables.
Nursing and medical neglect are as serious as active abuse and can have equally devastating consequences. Our nursing home neglect attorneys specialize in identifying and addressing various forms of neglect within nursing facilities.
Neglect differs from abuse in its passive nature but can be just as harmful. It includes failing to provide necessary care, leading to adverse patient outcomes. Various forms of neglect, from medical to basic needs, can significantly impact the resident's health and well-being.
Holding Nursing Homes AccountableOur firm is dedicated to holding nursing homes accountable for their actions. We rigorously investigate claims of nursing home abuse and neglect, determining the extent of the nursing home's liability and seeking justice for the victims.
Caregiving homes are legally responsible for providing patients with a safe and caring environment. Our attorneys assess whether nursing facilities have met their obligations and pursue legal action against those who fail to do so.
A Nursing Home's Role and LiabilityCaregiving homes have a legal and moral obligation to provide adequate patient care. Our nursing home abuse and neglect law firm examines the role and liability of nursing care homes in neglect cases, ensuring that the facility and its insurance company that fail to meet their obligations are held accountable.
Preventative MeasuresPreventing abuse is as important as addressing it after it occurs. Our firm advocates for proactive measures to safeguard the well-being of each elderly person in nursing homes.
Strategies to prevent abuse include:
- Regular monitoring of the nursing home
- Understanding patients' rights
- Knowing the signs of abuse or neglect
When physical abuse, emotional trauma, or mistreatment occurs, legal recourse is available to hold every responsible party accountable and seek compensation for victims. Our nursing home abuse lawyers guide clients through this process.
Understanding the types of damages and compensation available in neglect and abuse cases is crucial. Our legal representatives assist clients in filing claims, pursuing legal action, and ensuring they receive fair compensation for their suffering.
Nursing Home Law Center, LLC's CommitmentWitnessing abuse or neglect by the nursing home staff or others can be heartbreaking and infuriating. We at Nursing Home Law Center, LLC are prepared to help you navigate these turbulent waters with a free consultation and represent you on a contingency fee agreement. Call our nursing facility abuse lawyer at (800)926-7565 to ensure your loved ones receive the justice they deserve.
 Knox County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
Knox County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
