legal resources necessary to hold negligent facilities accountable.
Fontana Nursing Home Abuse Lawyer
 Elder abuse in nursing homes is a significant problem, with many instances going unreported due to fear or inability to communicate. This abuse ranges from physical harm to emotional and financial exploitation.
Elder abuse in nursing homes is a significant problem, with many instances going unreported due to fear or inability to communicate. This abuse ranges from physical harm to emotional and financial exploitation.
Nursing Home Law Center, LLC's experienced nursing home abuse lawyers are committed to uncovering and addressing these cases. Our firm supports victims and their families, advocating for their rights and working towards meaningful resolutions.
Legal Support for Victims of Nursing Facility Neglect and AbuseExpectations for quality care in nursing homes are high, yet the stark reality often includes instances of abuse and neglect, especially in areas like Fontana. Our Fontana nursing home abuse lawyer team is committed to addressing these injustices, emphasizing the right to compensation for victims of nursing home abuse or neglect.
Families trust professional caregivers, expecting their elderly loved ones to be treated with respect and dignity. Our legal team is dedicated to bringing justice and support to these victims, ensuring they receive the compensation and care they deserve.
Understanding Nursing Home Abuse and NeglectNursing facility abuse and neglect encompass a broad spectrum of harmful actions directed towards elderly residents, all of which violate their personal rights and run contrary to California law and public health standards. In Fontana, within San Bernardino County, these forms of abuse take various distressing shapes, including physical, emotional, sexual, and financial abuse.
Identifying and addressing these injustices is a critical role played by our Fontana nursing home abuse lawyers who tirelessly advocate for victim rights. Family members must be aware of the signs associated with these forms of abuse and know when to seek appropriate legal representation.
- Physical Abuse: Includes unexplained injuries such as bruises, cuts, or broken bones, often inadequately accounted for by nursing home staff members.
- Emotional Abuse: Signs of emotional abuse manifest as depression, withdrawal, or fear, especially when certain nursing home staff members or fellow residents are present.
- Sexual Abuse: Indications of non-consensual sexual contact characterized by physical signs or sudden and concerning changes in behavior.
- Financial Abuse: Watch for unexplained withdrawals from bank accounts, alterations in wills, or the disappearance of personal belongings.
- Neglect: Signs of neglect are evident in poor hygiene, malnutrition, or untreated medical conditions, indicating a lack of proper care, which may result from negligence or medical malpractice.
Identifying the signs of abuse and neglect is crucial in protecting the well-being of nursing home residents. Key indicators that someone may be a victim of emotional or physical abuse or neglect in a nursing or assisted living facility include the following:
- Unexplained Injuries: Bruises, cuts, or fractures that cannot be adequately explained.
- Sudden Behavioral Changes: Withdrawal, fear, or anxiety that was not present before.
- Poor Hygiene: Indications that basic personal care is being neglected.
- Weight Loss: Unexplained or sudden weight loss can signal neglect or abuse.
- Overmedication: Signs that the resident is being improperly medicated.
When abuse or neglect is suspected in a caregiving home or assisted living facility, taking immediate and decisive action is essential. The first step should always be to ensure the safety and well-being of the resident, which may involve seeking medical attention. Reporting the incident to the authorities, including social services and law enforcement, is also critical.
As Fontana caregiving home lawyers, we advise documenting all signs and incidents of abuse or neglect, as this evidence is crucial in any subsequent legal proceedings. Our firm can guide you through the process of evidence-gathering and legal representation.
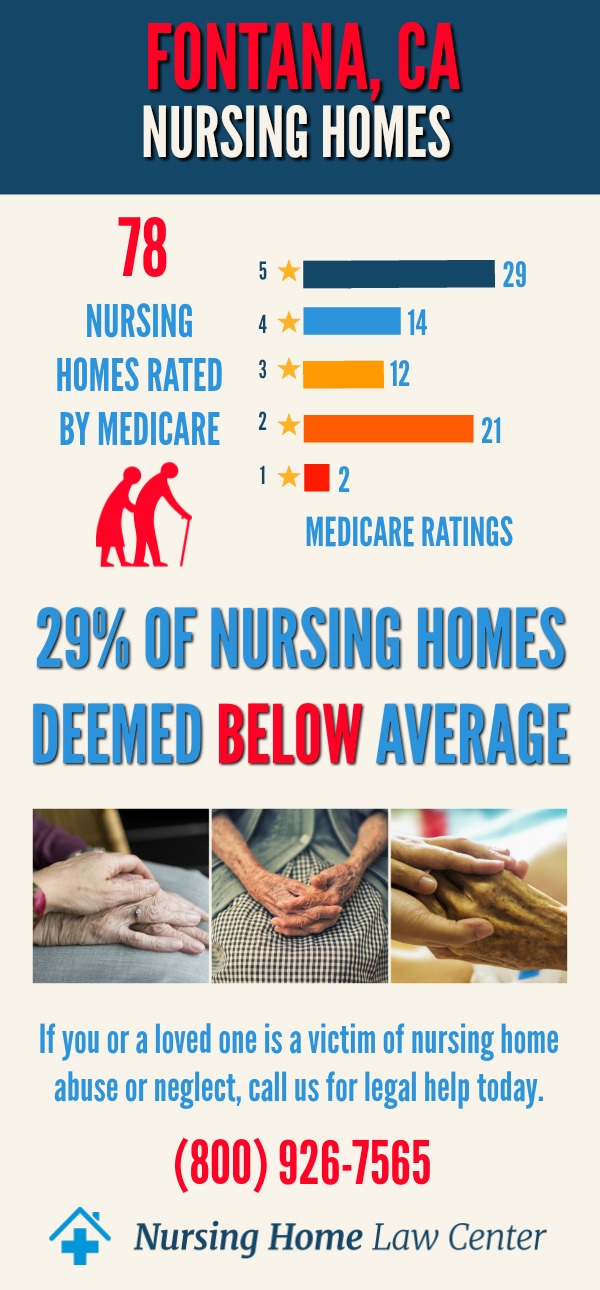
Nursing Facility Abuse StatisticsAbusive behavior is a significant issue nationwide, and the statistics paint a concerning picture. Nationally, reports indicate a high prevalence of abuse and neglect in eldercare homes and assisted living facilities. In California, similar trends are observed, with numerous cases reported annually. We specialize in nursing home abuse cases and use these statistics to inform our strategies and advocate effectively for our clients.
In December 2023, a report from the Centers for Medicare and Medicaid Services (CMS) shed light on the state of caregiving facilities in Fontana, California. The findings were stark and concerning, revealing that out of the 88 caregiving homes assessed in the area, 27, which amounts to 31%, were rated as "below average" or "much below average."
This revelation underscores the pressing need for vigilance and advocacy in ensuring the well-being and safety of elderly residents in Fontana's nursing facilities.
Seeking Compensation for Abuse or NeglectAs experienced nursing home lawyers, we work diligently to ensure our clients receive the justice and compensation they deserve. Our approach involves:
- Thorough analysis of the case
- Evidence gathering
- Strategic legal representation
Abused victims may be entitled to various forms of compensation. Economic damages cover tangible losses such as medical bills and costs related to the abuse or neglect. Non-economic damages account for the more subjective impacts, like emotional distress, pain, and suffering.
Reporting Mistreatment: a Vital Step in Ensuring JusticeIn the pursuit of justice and protection for victims of negligence, mistreatment, or abuse within nursing care facilities, it is essential to grasp the critical steps involved and their significance. Timely reporting and adept legal support play pivotal roles in safeguarding the rights and well-being of vulnerable residents.
- Reporting Incidents: Swiftly alerting the appropriate authorities, such as the Ombudsman, is paramount in initiating protective measures for affected residents.
- Gathering Compelling Evidence: The foundation of a robust nursing home abuse case rests on the meticulous collection of evidence, encompassing medical records, eyewitness accounts, and other pertinent documentation.
- Thorough Documentation and Expert Testimony: The credibility and weight of abuse allegations are significantly bolstered through the meticulous documentation of incidents and the presentation of expert testimony.
- Navigating Settlements and Trials: Successfully navigating the legal avenues of settlements and trials requires the expertise and experience of a seasoned Fontana nursing home abuse lawyer.
While taking these critical steps, it's important to be aware of the available resources for reporting abuse, including:
- California Adult Protective Services
- California Advocates for Nursing Home Reform (CANHR).
- California Department of Public Health's Licensing and Certification Division
- California Long Term Care Ombudsman Program at (800) 231-4024.
- Division of Medi-Cal Fraud & Elder Abuse (DMFEA): (800) 722-0432.
- Elder and Dependent Adult Abuse Reporting Hotline: (888) 436-3600.
Our commitment to our clients' cases is unwavering. Our Fontana nursing abuse attorneys are recognized for their expertise, experience, and dedicated approach to handling abuse and neglect cases. We understand these cases' emotional and legal complexities and strive to provide compassionate and effective legal representation.
We dedicate ourselves to advocating for their rights and securing the compensation they need to move forward. If your family member has suffered bodily harm in a caregiving home, our elder abuse law firm is dedicated to seeking accountability.
Thanks to our contingency fee agreement, our proficient personal injury attorneys will pursue a civil lawsuit without any cost to you unless we win. Call our nursing home abuse lawyers at (800) 926-7565 for a free case evaluation to discuss your nursing home abuse case.
 San Bernardino County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
San Bernardino County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
