legal resources necessary to hold negligent facilities accountable.
Fayetteville Nursing Home Abuse Lawyer
 When you entrust the care of your loved one to a nursing home, you expect them to receive the care, dignity, and respect they deserve. Unfortunately, situations in nursing homes are not always ideal.
When you entrust the care of your loved one to a nursing home, you expect them to receive the care, dignity, and respect they deserve. Unfortunately, situations in nursing homes are not always ideal.
In 2020, the World Health Organization (WHO) found that 2 in 3 nursing home employees admitted to committing abuse in the past year. However, the study does not have data for cases reported by victims or their proxies. Hence, the rates of nursing home abuse may be higher than we think.
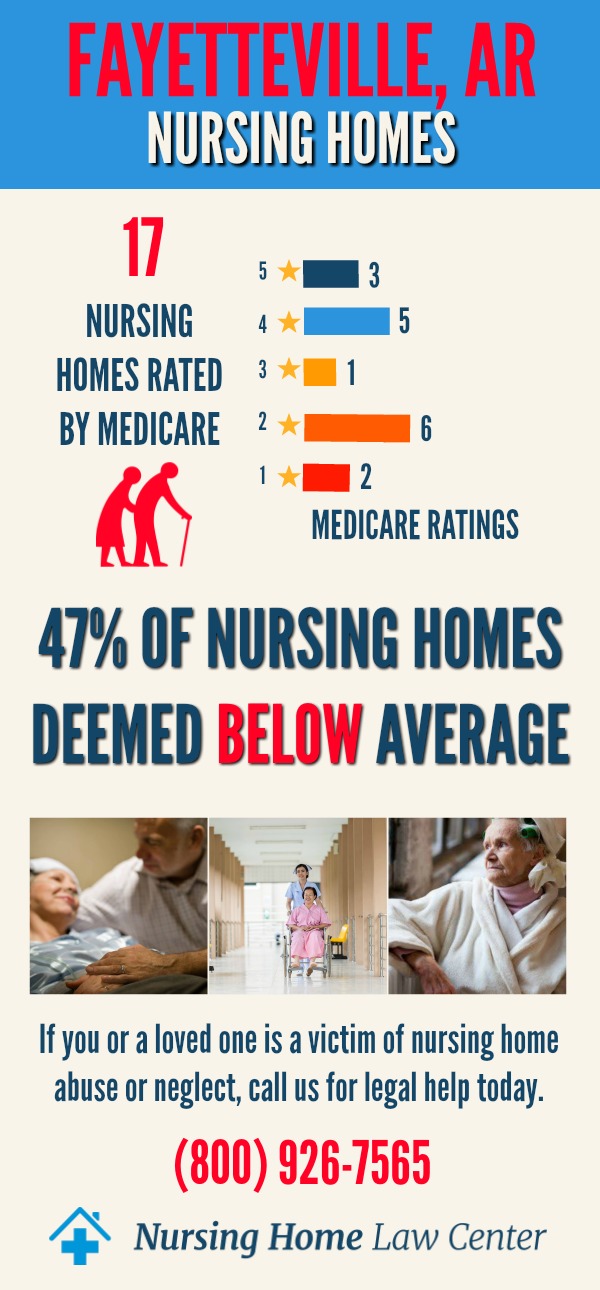
Do you suspect your loved one is experiencing abuse or subpar care in their Fayetteville nursing home? If so, the affiliate Arkansas personal injury attorneys at Nursing Home Law Center, LLC are ready to help.
Call our Fayetteville nursing home abuse lawyers at (800) 926-7565 (toll-free phone number) to schedule a free consultation. Our nursing home abuse attorneys will help you recover financial compensation for your damages through litigation or an out-of-court settlement-- you don’t pay unless we win.
What Is Nursing Home Abuse?Nursing home abuse is a single or repeated intentional act that causes a resident physical, psychological, or financial harm. It can result from negligence, carelessness, or malicious intent of employees, visitors, or other residents.
What Is Elder Abuse?The law defines elder abuse as a single or repeated act or lack of action that causes harm to a person aged 60 and above. The mistreatment of an older person is considered elder abuse if it occurs in a relationship with an expectation of trust.
Considering over 90% of nursing home residents are seniors, elder abuse is the most common type of abuse in nursing facilities.
Federal and State RegulationsThe federal and state governments implement laws to protect the welfare of residents in nursing home facilities. These laws include:
The 1987 Nursing Home Reform ActThe federal government created the 1987 Nursing Home Reform Act to define what services nursing homes must provide residents and to establish standards for these services. This law aims to protect the legal rights of nursing home patients, including:
- Freedom from abuse, neglect, or mistreatment
- Freedom from physical restraints
- Privacy
- Accommodation of physical, psychological, medical, and social needs
- Participation in resident and family groups
- Be treated with dignity
- Exercise self-determination
- Communicate freely
- Participate in one’s care plan review and be fully informed in advance about any changes in care, treatment, or status change in the facility
- Voice grievances without discrimination or reprisal
Similar rights are outlined in Chapter 10, Subchapter 12 of the Arkansas Code (§ 20-10-1204 - Residents' rights) in addition to the rights to:
- Be fully informed of the facility’s services and related charges before admission
- Examine results of inspections conducted by federal or state agencies
- Have copies of the rules and regulations of the facility and an explanation of individual responsibilities
- Manage financial affairs on one’s own or delegate that responsibility to the licensee but only to the extent of the funds held in trust
In 2021, the Arkansas Senate approved House Bill 1776, requiring nursing homes to provide an average of 3.36 hours of direct care to each resident per day. Previous laws only mandated an average of 2.8 hours of direct care per resident daily.
The law also requires one direct-care employee for every 14 residents during the overnight shift and one direct-care employee for every six residents during the day shift.
Types and Common Signs of Nursing Home AbuseKnowing what type of abuse your loved one is suffering from can help you determine the best way to help them. Nursing home abuse can take many forms, including:
Physical AbusePhysical abuse involves intentionally using force against a resident, causing injury, pain, or impairment. It includes but is not limited to actions like slapping, striking, kicking, burning, pinching, and restraining without medical reasons.
Signs of Physical Abuse
- Broken bones
- Unexplained injuries (e.g., cuts, burns, bruises)
- Broken eyeglasses
- Restraints or grip marks
- Fearfulness
- Post-traumatic stress disorder (PTSD)
Psychological abuse, also known as mental or emotional abuse, involves verbal and non-verbal acts that cause psychological harm to a resident. These acts may include verbal abuse, humiliation, intimidation, gaslighting, and geographical or social isolation.
Psychological Abuse
- Personality or behavioral changes
- Depression or anxiety
- Fearfulness
- Being extremely withdrawn
- Loss of enjoyment in usual activities
- Irritability
- Difficulty sleeping
Sexual abuse is any non-consensual sexual contact with another person. It can take many forms, including verbal sexual harassment, unwanted touching, sodomy, coerced nudity, and rape. Sexual contact with a person that cannot give valid consent (e.g., a minor or mentally-challenged person) is also regarded as sexual abuse.
Signs of Sexual Abuse
- Reluctance or refusal to be touched
- Unexplained bruises around the breasts or genitals
- Genital infections
- Sexually transmitted diseases
- Unexplained vaginal or anal bleeding
- Sudden changes in personality or behavior
- Refusal to be alone with specific individuals
Financial abuse is the illegal, unauthorized, or improper use of a resident’s personal property, including money and assets. Financial abuse occurs in different ways, such as cashing checks without permission, stealing valuables, and forging financial documents.
Signs of Financial Abuse
- Sudden bank account changes
- Unexplained transactions on credit cards
- Missing belongings
- Forged signatures on financial documents
- Inconsistencies in financial records of the facility
- Sudden changes in financial habits
Medical neglect occurs when nursing home staff fails to provide a patient’s basic needs, including food, medication, clothing, medical care, and a clean environment, creating or increasing the risk of harm to a patient.
On the other hand, emotional or social neglect is the failure to provide a patient with opportunities to fulfill social and emotional needs. Emotional neglect typically occurs through social isolation.
Signs of Neglect
- Poor hygiene
- Bed sores
- Malnutrition or dehydration
- Unexplained weight loss
- Untreated medical conditions
- Unsafe or unsanitary living conditions
- Inadequate clothing for the weather
- Poor mental health
- Lack of medical aids (e.g., eyeglasses, walkers, hearing aids)
- Overdosing or underdosing and other medication errors
Nursing home neglect and abuse are not always noticeable. Despite warning signs, abusers may attempt to hide them from the victim’s family members or blame unexplained injuries on an unrelated cause. Moreover, the indicators of abuse and neglect may be similar to dementia or mental illness.
That said, families must be wary of the common signs of abuse and how they differ from normal aging, mental illness, and dementia. For instance, elder abuse and dementia share similar indicators, such as memory loss, mood changes, and self-neglect.
Consult a specialist about your loved one’s health concerns. At the very least, a doctor should be able to rule out medical explanations for your loved one’s injuries or behavioral changes.
Who Is Most at Risk?Many residents have a certain level of risk of abuse and neglect. However, some individuals are more vulnerable than others, including:
- Patients with physical or mental disabilities
- Patients that require additional medical care
- Patients with access to an abundance of wealth
- Dementia patients
- Women and children
- Bedridden patients
Victims often suffer severe and long-term consequences of nursing home abuse and neglect, such as:
- Physical injuries
- Untreated medical conditions (e.g., bed sores)
- Psychological trauma
- Emotional distress
- Property and monetary losses
- Loss of quality of life
- Reduced family or social ties
- Increased risk of illnesses
- Wrongful death
The factors that lead to the abuse of disabled or elderly residents include:
- Underqualified and Improperly Trained Staff Members: Nursing home facility employees require proper qualifications, training, and experience to care for disabled and elderly residents. Without an adequate background, employees may be likelier to commit mistakes or engage in abusive behavior.
- Understaffing: Not having enough staff members to care for all residents increases the risk of abuse and neglect. Understaffing also makes it challenging to abide by the “3.36 hours of direct patient care per day” rule in Arkansas law.
- Poor Management: Disorganization, lack of accountability, and substandard supervision may create irresponsible, abusive, or disgruntled staff members, increasing the risk of mistreatment among residents.
- Lack of Background Checks: Failure to screen applicants for histories of abuse or neglect may put residents’ well-being in danger.
- Underreporting: Unfortunately, many nursing home abuse cases remain unreported. Hence, abuse and neglect often go unresolved in many nursing facilities.
Report known or suspected abuse to the Fayetteville Police Department as soon as possible. The police will investigate your claims and take proper action, possibly including the filing of criminal charges against the abuser.
Call 911 if you think your loved one or another nursing home resident is in immediate jeopardy.
You can also file a report to the following Arkansas agencies:
- Adult Protective Services
- Long-Term Care Ombudsman
- Division of Aging and Adult Services
- Office of Attorney General
State and local agencies may suspend or revoke the licenses or certifications of Fayetteville nursing homes found guilty of abuse or neglect.
After you file a complaint to the proper authorities and remove your loved one from the dangerous situation, call an attorney for formal legal advice regarding your situation.
Filing a Fayetteville Nursing Home Abuse ClaimEvery nursing facility has the legal obligation to ensure its residents are in good health and free from any kind of mistreatment. Similarly, every staff member is responsible for ensuring that all their charges receive adequate care. A claim or lawsuit may be in order if a nursing home or its constituents fails to meet these obligations and a resident suffers harm.
Did you or a family member suffer physical, financial, or mental harm due to the negligence of a Fayetteville nursing home? If so, you could hold the facility accountable by filing a personal injury claim.
The Role of Your Nursing Home Abuse LawyerFiling a claim without legal help may jeopardize your chances of recovering a fair settlement. Thus, you should hire an experienced personal injury attorney who can help you:
- Establish the liability of at-fault parties
- Collect evidence to support your claim
- Handle all claim-related paperwork
- Negotiate settlement values
- File your case in civil court, if necessary
When filing a claim, you must determine who is responsible for your damages. At-fault parties may include:
- Nursing home staff members
- Visitors
- Other nursing home residents
The nursing home owner or administrator may also be held accountable for failing to protect its residents, regardless of who is directly at fault for the abuse or neglect.
EvidenceSubstantial evidence is crucial to prove the liability of a negligent nursing facility. Your personal injury attorney will help you gather evidence, including:
- Photos of your loved one’s injuries
- Medical records, including psychological evaluations
- Incident and police reports
- Financial records
- Witness accounts from employees, visitors, or other nursing home residents
- Proof of understaffing, lack of supervision, or similar conduct
- Expert testimony
Filing a personal injury case against your loved one’s nursing home could help you recover financial compensation for the following economic and non-economic losses:
- Medical Expenses: Compensation for your loved one’s medical bills, including hospitalization, medication, therapy, surgery, emergency transportation, etc.
- Disability: Compensation for disability-related damages if your family member becomes disabled from the abuse or neglect. These damages may include loss of quality of life and medical equipment.
- Pain and Suffering: Compensation for physical and non-physical injuries from physical or emotional abuse, including physical pain, mental trauma, emotional distress, etc.
- Loss of Quality of Life: Compensation for your loved one’s reduced quality of life after the abuse or neglect, which may manifest in loss of enjoyment in daily activities, decreased independence, reduced societal ties, etc.
- Wrongful Death: Compensation for death-related damages if your loved one dies due to abuse or neglect. These damages typically include funeral and burial costs, pre-death medical treatment, grief, etc.
- Punitive Damages: Monetary awards on top of compensatory damages, aiming to punish negligent nursing homes for their actions and deter harmful behavior in the future.
After you file a personal injury case against the nursing home, the facility’s insurance company may offer you a settlement. You can accept the initial offer, but you will no longer be able to sue for additional damages.
Unfortunately, not all insurance companies offer fair settlements to nursing home abuse victims. You should consult a lawyer first before taking the offer.
LitigationYour Fayetteville nursing home abuse lawyer can negotiate the settlement offer on your behalf. However, if the nursing home refuses to make a better offer or denies liability for the mistreatment, you could file a case in civil court.
When you file a civil lawsuit, a judge or jury will hear both sides of the story to determine a verdict. Depending on the case's complexities, this process could last between a few hours and a few months. An appeal may be possible if a party is dissatisfied with the result.
Your Fayetteville nursing home abuse lawyer can also walk you through other legal options, such as mediation or arbitration.
The Statute of Limitations in ArkansasThe statute of limitations for personal injury cases is three years from the date of the underlying incident or injury (Arkansas Code § 16-56-105). If the victim dies, the statute of limitations is three years from the date of death.
Taking legal action as soon as possible is crucial to obtaining a fair settlement. Missing the deadline could render your nursing home abuse case useless. And if you still file a lawsuit outside the statute of limitations, the defendant will likely file a motion to dismiss.
How to Prevent Nursing Home Abuse and NeglectFamily members of nursing home patients can help prevent abuse and neglect by:
- Making frequent visits
- Observing how employees treat residents
- Learning the difference between signs of abuse and normal aging, mental illness, or dementia
- Watching for strange injuries or behaviors in their loved ones
- Checking for violations made by the facility
- Encouraging their loved ones to talk about their negative experiences in the nursing home
- Talking to other residents about their experiences
- Giving loved ones a means to contact the family in emergencies
- Getting to know their loved ones’ primary caregivers
- Reviewing facility records for inconsistencies and unauthorized transactions
- Checking loved ones’ bank accounts regularly
Most importantly, families must take legal action against negligent facilities once they find evidence of abuse or neglect. Apart from recovering financial compensation, a facility that faces financial repercussions could start making changes to prevent mistreatment from reoccurring.
Avoid giving nursing facilities the benefit of the doubt. Act as soon as possible if you think your loved one suffers from abuse, neglect, or mistreatment.
Schedule a Free Consultation With an Expert Fayetteville Nursing Home Abuse LawyerNursing homes owe all residents proper care and protection from abuse, neglect, and other forms of mistreatment. Failure to do so counts as a violation of the law, making way for a legal claim or lawsuit.
The nursing home abuse lawyers at Nursing Home Law Center work tirelessly to defend victims’ legal rights and hold negligent nursing homes liable for their actions. Filing a claim or lawsuit with the help of one of our Fayetteville nursing home abuse attorneys could help you recover compensation for your medical expenses, injuries, mental trauma, and other losses.
Our affiliate skilled nursing home abuse lawyers handle all accepted nursing home abuse cases on a contingency basis, meaning our services are free unless we win.
Call our law offices at (800) 926-7565 or use this contact form for a free case evaluation. All information you share with our Fayetteville nursing home abuse attorneys will remain confidential under an attorney-client relationship.
Resources: Washington County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home
Washington County Nursing Home Injury Lawyer Nursing Home Law Center LLC Home