legal resources necessary to hold negligent facilities accountable.
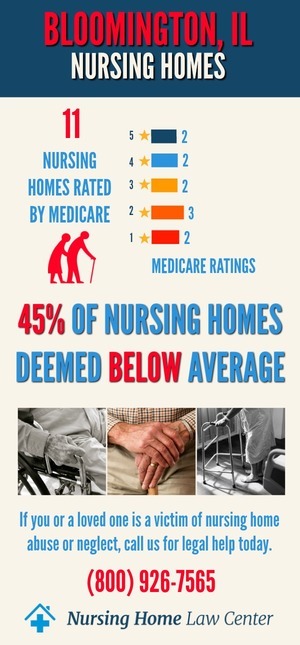
Bloomington Illinois Nursing Home Abuse Lawyer
 Every resident in an Illinois nursing facility is at risk of being abused, mistreated, or neglected. Without the immediate intervention of family members, friends, or other staff members, the victim could suffer serious injuries or death
Every resident in an Illinois nursing facility is at risk of being abused, mistreated, or neglected. Without the immediate intervention of family members, friends, or other staff members, the victim could suffer serious injuries or death
Is your loved one a victim of nursing home abuse? The affiliate Illinois personal injury attorneys at Nursing Home Law Center, LLC are legal advocates who fight for residents' rights and provide matchless legal services.
Contact our Bloomington nursing home abuse lawyers at (800) 926-7565 to schedule a free consultation to discuss your case. All confidential or sensitive information you share with our legal team remains private through an attorney-client relationship policy of our law firm.
What Is Nursing Home Abuse?Nursing home abuse is defined as any mistreatment that causes harm of injury to a resident. Nursing home abuse can take many forms, including physical, emotional, sexual, and financial abuse. Neglect is also considered abuse since it can lead to serious injuries and even death.
Nursing home abuse is shockingly common. WHO (World Health Organization) data shows that two out of three staff members admit to abusing elderly residents. The elderly are highly susceptible to abuse because they:
- Depend on the Staff: Since residents of nursing homes and long-term care facilities rely on the staff for their basic needs, they are more vulnerable to abuse.
- Are Isolated: Residents in nursing homes can be isolated from family and friends, making it harder for them to report abuse.
- Have Dementia or Alzheimer’s: Many nursing home residents have some form of dementia, which can make it difficult for them to communicate what is happening.
- Are Physically Weak: The elderly are often physically frail, making it difficult to defend themselves from abuse.
Nursing home residents may experience different types of abuse, including physical, emotional, sexual, financial, and neglect.
Physical Abuse
Physical abuse in a nursing home setting is any type of force that results in injury to a resident. It includes hitting, shoving, kicking, punching, biting, burning, or harming a resident.
Force can also be used to restrain a resident against their will. For example, if a staff member ties a resident to their bed or wheelchair without proper authorization, this is considered physical abuse.
Physical abuse also includes giving residents medication that is not prescribed for them or withholding necessary medicines.
Signs of Physical Abuse
Some physical signs of abuse are:
- Bruises, Cuts, Unexplained Injuries, and Broken Bones: A resident who is physically abused may have bruises in various stages of healing. They may also have cuts or broken bones.
- Burns: The resident may have burns from cigarettes, scalding water, or chemicals.
- Head Injuries: Head trauma is one of the most common fall-related injuries, especially if the resident is pushed off the stairs or on an elevated surface.
- Sprains and Disruptions: The resident may have sprains, dislocations, or internal injuries that are the result of being physically abused.
Emotional Abuse
Emotional abuse is any type of verbal or nonverbal attack on a nursing home resident that causes psychological harm. It includes:
- Yelling
- Name-calling
- Threatening
- Intimidating behavior
- Isolating
- Humiliating
- Blaming
- Ignoring
- Making faces
- Rejecting
- Intruding on personal privacy
Signs of Emotional Abuse
Some common signs of psychological abuse are:
- Withdrawal from Daily Activities: When someone is emotionally abused, they may start to withdraw from the activities they once enjoyed. They may also become more withdrawn and less communicative overall.
- Changes in Mood or Personality: The victim of emotional abuse may exhibit sudden changes in mood or personality, such as depression, anxiety, fearfulness, or agitation.
- Sleep Disturbances: Emotional abuse can cause sleep disturbances, such as insomnia or sleeping more than usual.
- Loss of Appetite: The victim may lose their appetite or only eat certain foods.
- Self-Harm: The victim may start to self-harm, such as cutting or burning themselves, to cope with the emotional pain they are feeling.
Sexual Abuse
Senior citizens in nursing homes also experience sexual abuse. Sexual abuse is any type of sexual contact or behavior that occurs without the victim's consent. It includes:
- Rape
- Attempted rape
- Unwanted touching or groping
- Voyeurism
- Exposing oneself
- Forcing the victim to watch or participate in sexual acts
Here are some common signs that a resident may have been sexually abused:
- Bruises on Genital Areas: Bruises or marks on the breasts, inner thighs, or genital area may signify sexual abuse.
- STDs: If the victim has contracted a sexually transmitted disease, this may be an indication that they have been sexually assaulted.
- Anal or Vaginal Bleeding: Bleeding from the anus or vagina can be a sign of rape or attempted rape.
- Depression or Anxiety: The victim may exhibit signs of depression or anxiety after being sexually abused.
Financial Abuse
Financial abuse is when someone illegally or improperly uses a nursing home resident's money or property. It includes:
- Forging the Resident's Signature: The abuser may forge the resident's signature on documents, such as checks to gain access to their money.
- Stealing the Resident's Money or Property: The abuser may steal the resident's cash, credit cards, checks, jewelry, or other valuables.
- Coercing the Resident to Sign Documents: If someone coerces a resident into signing documents, such as a will, power of attorney, or deed to their home, it is considered financial abuse.
- Using the Resident's Money or Property Without Consent: One of the staff members or other residents may use the victim's money or property without their consent. For example, they may use the victim's credit card to make purchases or take money from their bank account.
Signs of Financial Abuse
Family members may notice the following if their loved one in a nursing home is being financially exploited:
- Unusual Transactions: Any unusual transactions, such as large withdrawals from the victim's bank account may signify financial abuse.
- Changes in Financial Documents: If you see changes in the victim's financial documents, such as a new power of attorney or deed to their home, this may indicate that the resident is being taken advantage of financially.
- Unpaid Medical Bills: When the resident's medical bills are not being paid, even though there is money in their account to cover them, it may signify financial exploitation.
Nursing Home Neglect
Nursing home neglect means the staff is not providing proper treatment to the resident. Besides substandard care, nursing home neglect also includes:
- Not providing the resident with enough food or water
- Not providing proper medical care
- Not keeping the resident's living area clean
- Inadequate supervision
Signs of Nursing Home Neglect
Here are some signs that may indicate a nursing home resident is being neglected:
- Bed Sores: Bed sores develop due to a sedentary resident not being moved enough. If an elderly person stays in the same place for too long, they can develop pressure ulcers and bedsores. Pressure wounds can be very painful and may complicate a resident's existing medical conditions.
- Malnutrition: If residents are not getting enough to eat or drink, they may become malnourished. This can lead to weight loss, weakness, and dehydration.
- Poor Personal Hygiene: Lack of proper hygiene care results in skin infections and body odor.
Medical Malpractice
Although medical malpractice is a separate issue from elder abuse, it can still occur in nursing homes. Medical malpractice is when a healthcare professional provides subpar care that results in injury or death to the patient. It can include:
- Misdiagnosis: If the doctor fails to properly diagnose a resident's condition, it can result in serious health complications or death. It may also cause medication errors since the patient might get the medications they don't need.
- Inefficient Medical Care: Patients in long-term care facilities can be more vulnerable to developing infections. If the staff does not properly clean the resident's living area or take precautions to prevent the spread of infection, things can quickly go out of hand, harming multiple residents.
- Overmedication: Typically, overmedicating a nursing home patient can result in serious health complications, such as organ damage or heart failure. Medication errors are a serious matter since they can be lethal.
Any assisted living facility or nursing facility resident may be susceptible to abuse or mistreatment. However, certain residents may be more likely to be abused than others. These include residents:
- Suffering from Cognitive Impairment: Patients with dementia or Alzheimer’s may be more likely to be abused than those without cognitive impairments. They may be confused and vulnerable, unable to communicate what is happening to them.
- Having a Physical Disability: Residents unable to move around on their own or who require help with activities of daily living (such as eating, bathing, or using the restroom) cannot defend themselves or escape from an abusive situation.
- With History of Abuse: People with a history of abuse and trauma typically have a harder time trusting people. So, they may be reluctant to report abuse, fearing they will not be heard or believed.
- From a Minority Group: Unfortunately, minority groups are often targeted for abuse, whether it is due to racism, homophobia, or other forms of discrimination.
A nursing home is supposed to be a safe environment for your elderly loved one to spend time in while you cannot be with them or provide the care they need. Unfortunately, this is not always the case.
Nursing home abuse is a problem that affects far too many people every year, resulting in injuries and even death.
Here are some reasons that may cause this otherwise safe environment to become abusive:
- Inadequate Training: Nursing home staff must be properly trained to provide the best possible care for residents. Unfortunately, many facilities do not adequately train their employees or provide adequate resources. Inadequate training means the staff is unaware of how to care for residents properly or are overworked and stressed, leading to an increased risk of abuse.
- Lack of Staff: Employees may feel overwhelmed and overworked if there's not enough nursing home staff. It can lead to them taking out their frustration on residents. Additionally, with insufficient staff, residents may not get the individualized attention they need and deserve, which can also lead to abuse.
- Poorly Paid Employees: Employees who are paid poorly may feel disgruntled and underappreciated. As a result, they may not be able to provide the best care to residents.
- Lack of Supervision: Administrators and supervisors in a nursing home must ensure that the residents are getting proper care and attention. However, there is no supervision in many nursing homes. Due to this, there's no disciplinary action against abusive staff members.
Abuse in nursing homes can be prevented by taking specific measures. First, it's essential to train the staff properly about disease control, elder care, infection prevention, and proper lifting techniques. The staff should get regular check-ups and be up-to-date on their vaccinations.
Second, make sure that there are enough staff members on duty to provide adequate care. If the nursing facility is understaffed, it's more likely that abuse and neglect will occur.
Supervisors or administrators should conduct regular inspections of the facility and its residents. They should ensure the residents are being cared for properly. They should also create a zero-tolerance policy for any type of abuse or neglect.
Plus, they must encourage family and friends to visit often and report any concerns they have about the care their loved one is receiving. Unfortunately, many families are reluctant to speak up. Thus, the nursing home administration needs to provide a safe and welcoming environment for them to do so.
How to Report Abuse Suffered by Nursing Home ResidentsIf you or a loved one has been a victim of nursing home neglect or abuse, you should report it immediately. Unfortunately, many nursing home abuse cases go unreported, which means most residents don't get the justice they deserve.
When you speak up for yourself or your loved one, you don't only do them a favor but also protect other residents from abuse in nursing homes. Here's what you should do:
Report to the Administration
First off, report the abuse to the nursing home administrator. If they have a process for handling such complaints, follow it. Unfortunately, some nursing home administrators may downplay or ignore your concerns.
If that happens, don't give up. Instead, you should take your complaint to the next level by contacting the state's long-term care ombudsman.
Contact the State's Long-Term Care Ombudsman
The ombudsman is a state official who advocates for nursing home residents. They can help you file a complaint and investigate the abuse allegations.
For instance, you can consult the Illinois Department of Public Health to find the ombudsman in your state. The Illinois Department of Public Health is responsible for investigating complaints about nursing homes in the state.
You can also visit the National Long-Term Care Ombudsman Resource Center to find your state's ombudsman program contact information.
Contact the Police
In some cases, abuse in nursing homes can delve into the category of crime. Some examples include sexual assault and financial exploitation. You should contact the police and report the incident immediately.
File a Lawsuit
You can also file a lawsuit against the nursing home. It is usually a last resort, but it's an option if you feel like you've tried everything else and you're not getting anywhere.
A Bloomington nursing home abuse lawyer can help you file a lawsuit and get the compensation you deserve. Schedule a free consultation with our Bloomington nursing home abuse lawyer today to discuss your case.
How Can a Bloomington Nursing Home Abuse Lawyer Help?If you see any unexplained injuries or other signs of abuse on your elderly loved one, you should immediately bring the matter to the nursing facility's administration. Abuse, if ignored for too long, can become life-threatening.
It is best to pursue justice by working with a nursing home abuse attorney. A nursing home lawyer can help you in the following ways:
Make Sense of the Legal Process
Although the Illinois Department of Public Health and other state authorities have many regulations for protecting nursing home residents, the process for filing a complaint and taking legal action can be confusing.
A lawyer can help you understand your options and work with authorities to get your loved one the protection they deserve.
Gather Evidence
To win an abuse case, you will need to prove that the abuse occurred and that the nursing home or its employees are responsible. A personal injury lawyer can help you gather evidence, including eyewitness testimony, photographs, and medical records.
Get Compensation for Your Loved One
If your loved one has been the victim of nursing home abuse, they may be entitled to compensation. It can include money for their medical bills, pain and suffering, and other damages.
The nursing facility may also be required to pay non-economic damages, such as:
- Loss of Consortium: Consortium means the companionship, love, and affection between family members. Since serious abuse, such as fall-related injuries or medication errors, can result in death, it would cause loss of consortium for the resident's family.
- Emotional Distress: The victim may also be able to recover damages for the emotional anguish caused by the abuse, such as anxiety, depression, and fear.
- Punitive Damages: In some cases, the court may award punitive damages to punish the nursing home for negligence or intentional misconduct.
A nursing home lawyer can help you understand what types of compensation you may be entitled to and fight for the full amount you deserve.
File for Wrongful Death
If you lost your family member due to nursing home abuse, you may be able to file a wrongful death lawsuit. A nursing home lawyer can help you understand your legal options and take the necessary steps to hold the responsible parties accountable.
Hiring a Lawyer to Prosecute a Bloomington Pressure Sore LawsuitThe Bloomington nursing home abuse attorneys at Nursing Home Law Center, LLC specialize in cases involving resident mistreatment. We carefully evaluate every circumstance involved in our client’s case and will provide various legal options after an initial consultation.
Our attorneys make every effort possible to ensure that your loved one receives the proper care and attention. If our network of attorneys determines negligence or mistreatment was involved, we fight aggressively to ensure that you and your loved one receive the fair and just compensation you deserve.
Contact our Bloomington, IL law offices today at (800) 926-7565 or use the contact form to schedule a free case evaluation. Every bedsore nursing home abuse case we accept is handled through contingency fee arrangements. This agreement ensures you and your loved one receive immediate legal representation without any upfront payment.
Resources:
 Chicago Attorney Nursing Home Law Center LLC Home
Chicago Attorney Nursing Home Law Center LLC Home
